News
Newswise — New York, NY —
A study of more than 100,000 men and women revealed that dietary gluten is not associated with heart disease risk in people without celiac disease. The findings also suggest that limiting whole grains as part of a low-gluten diet may increase the risk of heart disease in people who do not have celiac disease.
The study, led by researchers at Columbia University Medical Center and Massachusetts General Hospital/Harvard Medical School, was published online today in the BMJ.
“Gluten is clearly harmful for people with celiac disease,” said lead author Benjamin Lebwohl, MD, MS, assistant professor of medicine and epidemiology at CUMC, director of clinical research in the Celiac Disease Center at Columbia University and gastroenterologist at NewYork-Presbyterian/Columbia University Medical Center. “But popular diet books, based on anecdotal and circumstantial evidence, have pushed the notion that a low-gluten diet is healthy for everyone. Our findings show that gluten restriction has no benefit, at least in terms of heart health, for people without celiac disease. In fact, it may cause some harm if they follow a low-gluten diet that is particularly low in whole grains because those grains appear to have a protective effect against heart disease.”
Celiac disease is an autoimmune disorder where the ingestion of gluten, a protein found in wheat, rye, and barley, causes inflammation of the small intestine, preventing the absorption of nutrients. Over time, celiac disease can lead to other health issues, including heart disease, anemia, and osteoporosis. Celiac disease can be effectively treated with a gluten-free diet.
Celiac disease is estimated to affect about 1 in 100 Americans. Another segment of the population has a condition called non-celiac gluten sensitivity, in which gluten triggers some symptoms in the absence of celiac disease. However, estimates of the number of Americans with non-celiac gluten sensitivity vary widely. “Despite the relatively low prevalence of celiac disease and non-celiac gluten sensitivity, surveys suggest that about one-third of Americans are trying to cut down on gluten,” says Dr. Lebwohl. “This certainly benefits companies that sell gluten-free products. But does it benefit the public? That is the question we wanted to answer.”
To assess the effects of a low-gluten diet on heart health, Dr. Lebwohl and his colleagues analyzed diet and coronary heart disease data on 65,000 women in the Nurses Health Study and 45,000 men in the Health Professionals Follow-up Study, excluding anyone who had been diagnosed with celiac disease. Each participant filled out detailed diet questionnaires every four years, from 1986 to 2010. The participants were divided into five levels of estimated gluten consumption.
“We decided to look at heart disease because it’s a leading killer, and because it’s generally understood that heart health can be affected by diet,” said Dr. Lebwohl.
The researchers found that there was no association between gluten intake and risk of coronary heart disease, defined as fatal or non-fatal heart attacks. “Even those with the lowest amount of gluten consumption experienced the same rate of heart disease as those who were consuming the most gluten,” said senior investigator Andrew Chan, MD, MPH, gastroenterologist and Chief of the Clinical and Translational Epidemiology Unit in the Massachusetts General Hospital Division of Gastroenterology and associate professor of medicine, Harvard Medical School. “Based on our data, recommending a low-gluten diet solely for the promotion of hearth health does not appear warranted.”
In subsequent studies, the researchers plan to look at the effect of gluten intake on other health outcomes, including cancer and autoimmune disease.
The study is titled, “Long-term Gluten Consumption in Adults without Celiac Disease and the Risk of Coronary Heart Disease: Prospective Cohort Study.” The other contributors are: Yin Cao (Massachusetts General Hospital and Harvard Medical School, Boston, MA); Geng Zong (Harvard T. H. Chan School of Public Health, Boston, MA), Frank B. Hu (Harvard T. H. Chan School of Public Health, Brigham and Women’s Hospital, Boston, MA, and Harvard Medical School); Peter H.R. Green (CUMC); Alfred I. Neugut (CUMC); Eric B. Rimm (Harvard T. H. Chan School of Public Health, Brigham and Women’s Hospital, and Harvard Medical School); Laura Sampson (Harvard T. H. Chan School of Public Health), Lauren W. Dougherty Harvard T. H. Chan School of Public Health); Edward Giovannucci (Harvard T. H. Chan School of Public Health, Brigham and Women’s Hospital, and Harvard Medical School); Walter C. Willett (Harvard T. H. Chan School of Public Health, Brigham and Women’s Hospital, and Harvard Medical School); Qi Sun (Harvard T. H. Chan School of Public Health, Brigham and Women’s Hospital, and Harvard Medical School).
The study was funded by grants the National Institutes of Health (K24 DK098311, UM1 CA186107, UM1 CA167552, R01 HL035464, R01 HL060712, R01 HL034594) and by an American Gastroenterological Association Foundation Research Scholar Award.
The authors declare no financial or other conflicts of interest.
###
Researchers have discovered that a new anti-rejection drug that is gentler on the kidneys after liver transplant also reduces weight gain, which is common after surgery and can lead to serious complications for transplant patients.
Researchers from the Intermountain Medical Center Transplant Program in Salt Lake City, led a randomized, international multi-center study of more than 700 patients, which also included researchers from Northwestern University, Novartis Pharmaceuticals Corp., and Mayo Clinic.
For the study, researchers compared a new drug, Everolimus, to Tacrolimus, a routinely prescribed anti-rejection drug. Researchers found that transplant patients taking Everolimus gained less weight – and kept it off at one and two years after starting the drug.
Weight gain after liver transplantation can lead to serious complications and increase the risk of post-transplant metabolic syndrome, cardiovascular events, and kidney failure. Components of post-transplant metabolic syndrome include diabetes, obesity, high blood pressure, and abnormal fat and cholesterol blood levels, which can cause heart disease and related adverse events such as heart attack and stroke.
Researcher will present results of the study at the American Transplant Congress in Chicago on Tuesday, May 2. The study is also published in the American Journal of Transplantation.
After transplant, patients must take anti-rejection drugs so their immune systems don’t attack and destroy the transplanted organ. The research was originally undertaken to see if Everolimus is gentler on the kidneys than Tacrolimus, the most commonly prescribed immunosuppressant drug.
“Everolimus did have less impact on kidney function, and the Food and Drug Administration approved the drug based on that finding for use in liver transplant patients,” said Michael M. Charlton, MD, researcher and clinician from the Intermountain Medical Center Center Transplant Program, and the study’s lead author.
Early-stage research had shown Everolimus prevented weight gain in fruit flies and other animals, so the researchers wondered if that finding would hold in human subjects, as well.
To find out, they randomized a total of 719 patients between 25 and 35 days after liver transplant into three study arms. The first group of 245 patients received Everolimus and reduced dose of Tacrolimus; the second group of 243 received the usual dose of Tacrolimus and served as the control group; and the final group of 231 patients were prescribed only Everolimus to suppress their immune systems.
“We found that the two Everolimus groups in this study gained around 10 pounds less than patients in the tacrolimus arm,” said Dr. Charlton. “It used to be that rejection was a big deal and that was the most common cause of liver rejection or death. Now, the most common cause of death following liver transplantation is related to cardiovascular events and cancers, with kidney function increasingly important as well. Cardiovascular disease, cancers, and renal disease are driven in part by weight.”
The reduced weight gain was seen both one and two years after transplant.
Dr. Charlton said the second most-common reason people need liver transplant today is weight-related liver failure. “Since nearly everyone who receives a liver transplant gains weight after the surgery, this could be an easy way to avoid or limit the need for a transplant,” he said.
###
Newswise — ANN ARBOR, MI –
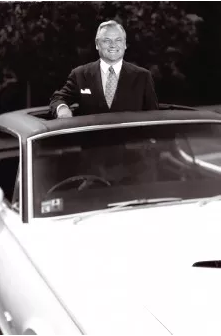
Fifty years ago this spring, entrepreneur Heinz Prechter moved his company to Detroit, to answer car buyers’ fast-growing demand for sunroofs. But even as his products brought light into more than a million vehicles, he fought darkness in his own life.
He struggled to keep his bipolar disorder hidden, until his suicide in July 2001 shocked the automotive industry.
Heinz’s wife, Waltraud “Wally” Prechter, resolved to fight the stigma that led her husband to hide his mental illness, and to address the lack of scientific understanding about the condition and how best to treat it. She channeled her energy into helping the University of Michigan Depression Center do both, by donating and raising money for a U-M bipolar research fund in her husband’s name.
Today, U-M named its entire bipolar disorder research program for Heinz Prechter, in honor of a new gift commitment of up to $5 million by the World Heritage Foundation - Prechter Family Fund.
But the gift comes with a challenge to others who care about bipolar disorder: The Prechter family will match every dollar given to U-M bipolar disease research up to $5 million. This will double the value of every donation, and the Prechter family gift will be available to researchers faster, if others step in to support the cause.
Donations can be made at http://victors.us/prechtercampaign.
Once the challenge is met, the Prechter family’s total giving to U-M bipolar research since Heinz Prechter’s death will be well over $10 million. Philanthropic gifts, including individual, foundation and corporate gifts, are critical to the effort and account for more than half of the research funding in any given year. The Prechter family set up this gift as a match to encourage more philanthropic support of research into bipolar disorder.
“I think that if you can — if you truly believe in something — you owe it to yourself to help, to give, and to make a difference. Because ultimately, that is all you leave behind,” says Wally Prechter.
Says U-M president Mark Schlissel, M.D., Ph.D., “I deeply appreciate Wally Prechter’s commitment to advancing bipolar disease research that will give hope to millions of people around the world. The Heinz C. Prechter Bipolar Research Program will enhance the University of Michigan’s longstanding research initiatives and drive new medical discoveries to combat this devastating disorder.”
Building new innovation and advancing bipolar science
“When we lost Heinz to his disease, it took Wally’s bravery and generosity to help us create incredible good out of such a tragic loss,” says John Greden, M.D., who was working with Heinz and Wally Prechter to create the U-M Depression Center at the time of Heinz’s death. Greden is the Depression Center’s director and a professor of psychiatry at Michigan Medicine, the U-M academic medical center.
“Without Wally Prechter’s leadership over the past decade, we would not have been able to develop the world’s first bipolar-specific stem cell lines, discover new genetic links, explore environmental factors or bring experts worldwide together as we have,” says Melvin McInnis, M.D., who is the Thomas B. and Nancy Upjohn Woodworth Professor of Bipolar Disorder, professor of psychiatry, and director of the newly named Heinz C. Prechter Bipolar Research Program.
The Prechter family is committed to increasing scientific understanding and treatment options that will enable people with bipolar disorder to lead healthy and productive lives. The new gift will grow the endowment that provides for the continuation of the Prechter Longitudinal Study of Bipolar Disorder, which has been ongoing for 11 years.
The Longitudinal Study allows researchers to track symptoms, response to treatment and overall health over time like never before. Already, more than 1,200 dedicated individuals have partnered with the research team to track personal and medical information for this long-term study.
“Our participants are the real heroes,” says Wally Prechter. “The goal of the Prechter Program is to identify effective solutions for people with bipolar disorder.”
Volunteers can also donate samples of their blood, giving scientists the chance to study tiny differences in DNA that may play a role in how the disorder develops, why it runs in families, how it affects people over time and what makes people vary in their response to treatment.
The “bank” of DNA from hundreds of research participants over the last decade is called the Heinz C. Prechter Bipolar Genetics Repository, and it is the nation’s largest privately funded bipolar genetics repository.
“We look forward to fueling new discoveries, and involving hundreds more people with bipolar and their families in the search for better treatments. The new funding, from the Prechters and others who believe in our work, will allow us to accelerate our pace of discovery,” says McInnis.
The Heinz C. Prechter Bipolar Research Program will be the umbrella program over the Longitudinal Study of Bipolar Disorder and other bipolar research studies.
About bipolar disorder
Bipolar disorder is a devastating, chronic mental illness with recurring episodes of mania (highs) and depression (lows). The illness causes unusual and dramatic shifts in mood, energy and behavior. Presently, 30 percent of individuals with bipolar disorder attempt suicide during their lives, and 20 percent die by suicide.
Although the direct cause of bipolar disorder is unclear, it has long been understood that genetic, biochemical and environmental factors play a role. Bipolar disorder runs in families, tends to recur throughout the life span and is affected by genes and life experiences.
Learn more about the entire Prechter-funded effort, and the research and team it has fueled, at http://www.prechterfund.org/. More information about participating in Prechter Bipolar Research Program studies is available by calling 1-877-UM GENES (1-877-864-3637) or emailing bpresearch@umich.edu.
Newswise — WASHINGTON, D.C., –
More than 100 radiation oncologists from across the United States are on Capitol Hill urging Congress to grow its investment in cancer research and to protect patients’ access to high quality cancer care. The doctors are in Washington to meet with Congressional leaders on Tuesday as part of the 14th annual Advocacy Day organized by the American Society for Radiation Oncology (ASTRO).
Radiation oncologists are emphasizing four priorities as they meet with policymakers and their staffers: (1) supporting cancer research by increasing the National Institutes of Health (NIH) budget by $2 billion; (2) avoiding disruptions in health insurance coverage for cancer patients; (3) preserving patients’ access to quality health care by stabilizing Medicare payments while pursuing innovative models of physician reimbursement; and (4) protecting access to radioactive isotopes. Infographics are available for each of these key issues.
Federal investment in cancer research has played a role in every major innovation in the fight against cancer and has led to a decline in the overall number of cancer deaths in the United States, yet funding for cancer research is under threat. The President’s proposed 2018 budget would cut $6 billion from the $32 billion earmarked for NIH, which could lead to a roughly 20 percent cut in the National Cancer Institute’s (NCI) budget. This drastic cut would derail the progress toward improved outcomes for cancer patients and cause leading scientists to leave the cancer research field. Cuts also would erase the commitment Congress made in late 2016 by passing the 21st Century Cures Act, which was widely-supported, bipartisan legislation that pledged nearly $5 million in additional support for the NIH.
“There are more than two hundred types of cancer, and only through research can we learn which treatments, including radiation therapy, will be most effective to fight the many different forms of this illness. We ask that Congress reject proposed cuts to federal cancer research funding and instead support an increase in the budget to eradicate cancer,” said Brian Kavanagh, MD, MPH, FASTRO, president of ASTRO and chair of the department of radiation oncology at the University of Colorado School of Medicine.
As Congress and the administration debate the future of American health care, ASTRO members are encouraging policymakers to prioritize reforms that avoid coverage disruptions for cancer patients. Studies have demonstrated that a lack of adequate health insurance leads to delayed diagnosis and treatment, resulting in higher mortality rates. Inadequate coverage also leads to higher costs that are felt throughout the economy. ASTRO strongly supports bipartisan solutions that protect cancer patients from losing their health insurance or not being approved for coverage following a cancer diagnosis, including maintaining bans on pre-existing condition exclusions and annual and lifetime caps; preserving guaranteed issue and guaranteed renewability provisions; and safeguarding access to clinical trials.
ASTRO members also are urging Congress to protect access to care by stabilizing Medicare reimbursement rates and fully supporting the transition to a health system that rewards quality over quantity. Congress unanimously passed the Patient Access and Medicare Protection Act in 2015, freezing payment rates for key radiation treatment services in freestanding clinics through 2018 at levels set in 2016 and requiring the Secretary of HHS to report to Congress on the development of alternative payment models (APMs) in radiation oncology. With the support of key Congressional leaders, we have much-needed stability in radiation oncology payments, and ASTRO has been working on the development of an APM that incentivizes adherence to nationally-recognized clinical guidelines through an episode-based payment framework across five primary cancer sites: breast, lung, prostate, colorectal, and head and neck. Radiation oncologists are on Capitol Hill to remind Congress of the multidisciplinary nature of cancer care and call for the opportunity to meaningfully participate in the nationwide transition to value-based health care.
“When Medicare inappropriately ratchets down on payments for cancer treatments, it jeopardizes whether patients have access to the care they need,” said David C. Beyer, MD, FASTRO, chair of the ASTRO Board of Directors and medical director of Cancer Centers of Northern Arizona at Sedona. “In the past decade, radiation oncologists in community-based practices have sustained as much as a 20 percent drop in their Medicare payments. We’re urging Congress to prevent additional cuts and support physician-led efforts to drive value-based care.”
Finally, ASTRO members are advocating to preserve access to radioactive isotopes. Any effort to abandon radioactive source-based technology in health care would limit patients’ access to certain radiation therapy treatments, which could interfere with treatment decisions and result in higher mortality and recurrence rates. A recent Nuclear Regulatory Commission analysis found no violations with safety or security consequences over the past 30 years, demonstrating the culture of safety and security among domestic radioisotope users. Moreover, radiation oncologists and medical physicists receive extensive training in the safe use and security of radioactive isotopes. ASTRO members are urging Congress to reject attempts to limit access to radioactive isotopes and promote policies that enhance the safe and effective use of these materials.
DIAGNOSING AND TREATING ALZHEIMER’S, DEMENTIA AT HOME COULD BE KEY FOR RURAL, LOW-INCOME POPULATIONS
Newswise —
Rural, older Floridians encounter a multitude of factors that put them at higher risk for developing Alzheimer’s disease (AD) such as limited education, decreased health literacy, low income, increased heart disease, lack of insurance, and limited access to health care. Minorities face an additional risk – African-Americans are nearly twice as likely and Hispanics are 1.8 times more likely than Whites to develop AD.
These disparities are especially prevalent in the culturally diverse, rural community of Belle Glade located in south central Florida in Palm Beach County, which has a higher percentage of residents over the age 65 (26.5 percent compared with the national average of 18 percent). More than one-third of the residents live below the poverty level. Belle Glade is designated as a Medically Underserved Area and a Health Professional Shortage Area for primary and specialty care.
With only two local physicians and two public primary care health clinics in the area, patients have to wait hours to see a health practitioner and cannot make appointments in advance. For older patients, this is a major barrier to seeking health care. Even if these rural older adults are aware of the need for cognitive assessment, there are insufficient providers to screen, diagnose, and treat the illness. These facilities are overwhelmed with waiting lists of patients needing appointments, and there are no urgent-care facilities available in the area. Consequently, residents treat the emergency room as the clinic.
Researchers from the Christine E. Lynn College of Nursing at Florida Atlantic University have received a $95,133 grant from the Ed and Ethel Moore Alzheimer’s Disease Research Program of the Florida Department of Health to test a novel mechanism in Belle Glade for early detection, diagnosis and treatment of AD in the home setting to reduce AD-related costs in underserved communities. The long-term goal of the study is to create a model for increasing early detection and treatment of AD that can be replicated in other underserved communities in Florida. A key outcome of this study is to delay earlier transitions to skilled nursing facilities, which could decrease health care costs by up to 30 percent for people with AD. Prior studies have shown that Medicaid can provide home care based services to three people for the cost of caring for one person in a long-term care institution.
“The lack of easily accessible, culturally proficient, and gerontology-trained providers creates a unique challenge for older adults in rural communities and really warrants further investigation,” said Lisa Wiese, Ph.D., principal investigator of the study and an assistant professor in FAU’s College of Nursing. “We anticipate that offering health care access to a nurse practitioner at either a rural clinic site or home health visit will be more effective than the current practice of waiting until symptoms develop. We also expect that home-based dementia screening and detection services will be more effective than screening and treatment at a local clinic.”
The study will examine a cohort of diverse rural residents’ perceptions and behaviors regarding health screenings and follow-up in the home as compared to a clinical setting and will compare the effectiveness of home-based or clinic screenings and follow-up evaluations. Gerontology-trained and culturally competent nurse practitioners will conduct dementia-specific geriatric assessments in individuals identified as being at risk through the home or clinic screening efforts. Continuing care management by a nurse practitioner will be provided. The researchers will pilot-test a referral program, “ROAD (Rural Older Adults with Dementia)-Next-Steps,” modeled after the Alzheimer’s Association Next Steps’ program of following patients after cognitive assessment to ensure that rural Florida residents receive continuing support as needed.
“Providing earlier cognitive assessment to facilitate earlier management of cognitive decline issues can assist with aging-in-place and decreased health care costs,” said Marlaine Smith, Ph.D., dean of FAU’s College of Nursing. “With more convenience, a less threatening environment and elimination of barriers like cost, transportation and long wait times, we can help individuals in rural areas live with greater independence at home and avoid admission to acute or long-term care institutions.”
In Florida, nearly 38 percent of individuals who have AD are undiagnosed, and more than 50 percent of Americans with dementia do not receive a cognitive assessment before they are institutionalized.
FAU’s College of Nursing is internationally known for its commitment to nursing as a discipline focused on nurturing the wholeness of persons and the environment through Caring. The College advances Caring knowledge through education, practice, research and scholarship to transform care locally, nationally and globally. Currently, the College of Nursing offers bachelor’s, master’s, DNP and Ph.D. degree programs with approximately 1,600 nursing students enrolled in its programs. For more information, visit www.nursing.fau.edu.
- FAU –
About Florida Atlantic University:
Florida Atlantic University, established in 1961, officially opened its doors in 1964 as the fifth public university in Florida. Today, the University, with an annual economic impact of $6.3 billion, serves more than 30,000 undergraduate and graduate students at sites throughout its six-county service region in southeast Florida. FAU’s world-class teaching and research faculty serves students through 10 colleges: the Dorothy F. Schmidt College of Arts and Letters, the College of Business, the College for Design and Social Inquiry, the College of Education, the College of Engineering and Computer Science, the Graduate College, the Harriet L. Wilkes Honors College, the Charles E. Schmidt College of Medicine, the Christine E. Lynn College of Nursing and the Charles E. Schmidt College of Science. FAU is ranked as a High Research Activity institution by the Carnegie Foundation for the Advancement of Teaching. The University is placing special focus on the rapid development of critical areas that form the basis of its strategic plan: Healthy aging, biotech, coastal and marine issues, neuroscience, regenerative medicine, informatics, lifespan and the environment. These areas provide opportunities for faculty and students to build upon FAU’s existing strengths in research and scholarship. For more information, visit www.fau.edu.
Newswise — ANN ARBOR, Mich. –
For medical student Katie Goldrath, the first time delivering difficult health news came when she had to tell a young woman named Robin and her mom, Delmy, that Robin had leukemia.
As she broke the news, Goldrath was conscious of not only her words but also her body language: Was she leaning in, looking the patient in the eye and expressing empathy?
The conversation, though, was just for practice.
Robin and Delmy were virtual humans on a computer screen — lifelike beings that are intelligent and conversational and have the capacity to interact using a wide range of communication behaviors shared in typical face-to-face dialogue.
Such intuitive interactions could help aspiring doctors better prepare for difficult and emotionally charged encounters with patients and hospital colleagues, according to a study recently published by researchers from Medical Cyberworlds Inc. and the University of Michigan in the international journal Patient Education and Counseling.
“Communication is the most important part of the doctor-patient relationship,” says lead author Frederick Kron, M.D., adjunct research faculty in the department of family medicine at the U-M Medical School and founder of Medical Cyberworlds, the company that developed the virtual reality program.
“We found that virtual human simulation was an engaging and effective tool to teach medical students advanced communication skills and, very importantly, that skills in the simulation transferred into a more realistic clinical situation.”
Research shows that poor clinician communication skills may contribute to lower levels of patient satisfaction, poorer health outcomes, and higher risk of complaints and malpractice claims. Poor communication is consistently among the most frequently identified root causes for sentinel events in hospital settings — events that can lead to preventable patient harm or even death.
“Finding an effective way to assess and teach advanced health care communication skills has been a long-standing challenge,” says co-author and U-M family medicine professor Michael Fetters, M.D. “Medical learners have a great need for practical, innovative methods to help them master the complexities of health care communication and develop excellent communication skills — both verbal and nonverbal. Ours is the first-ever research showing that it can be done effectively with virtual reality.”
Researchers addressed this challenge using revolutionary virtual human technology called MPathic-VR. This Medical Cyberworlds application allows learners to talk with emotive, computer-based virtual humans who can see, hear and react to them in real time. The virtual humans use a full range of behaviors expected between two people talking together.
The system assesses learners’ body language, facial expressions and communication strategies, then uses this information to produce real-time responses from the virtual human and provide personalized suggestions based on the learners’ strengths or weaknesses. Learners also see their interactions with the virtual human on video, then get the chance to apply what they’ve learned.
The carefully designed structure of the learning experience, including the repeat interactions, improved the students’ communication skills, the findings suggest.
Virtual practice, real benefits
The study was conducted among 421 students at three U.S. medical schools. Half the group used virtual reality, half used more traditional computer-based learning.
Goldrath, now in her fourth year of medical school at Michigan, says she benefited from the opportunity to practice scenarios in virtual reality, and the video feedback helped her understand how others might perceive her role and reactions.
“Many times, patients don’t initially absorb a doctor’s explanations because of shock, denial, fear or other emotions,” she says. “Factors like whether the doctor was standing over you or leaning in to comfort you, or whether he or she read from a piece of paper or looked you in the eye, leave a lasting impact on the patient. These actions represent to the patient what kind of support system the provider will be to him or her during these difficult times.”
Current teaching methods typically include small groups of learners and focus on role-playing with each other or with simulated patients. But this method, the study’s authors note, is very resource intensive, and different trainers may lead to discrepancies between groups.
Improving outcomes
As part of the study, students also practiced their interprofessional communication to learn the importance of effective dialogue on health care teams.
In that scenario, learners had to manage an interaction with a virtual oncology nurse who was angry that the student inadvertently omitted her from a family meeting with a patient she was caring for.
The virtual human communication system underscores the value of clear dialogue between and across health care teams in providing safe, effective patient care, the authors say.
“Health care has long needed innovative learning methods to better engage students in constructing knowledge and produce better learning outcomes,” says research collaborator Tim Guetterman, Ph.D., of U-M Family Medicine. “We are hopeful that, through our work, we have taken a significant step in that direction.”
Disclosures: Frederick Kron serves as president and Michael Fetters has stock options in Medical Cyberworlds Inc., the entity receiving grant funds for this project.
Newswise —
Johns Hopkins researchers report that an analysis of survey responses and health records of more than 10,000 American adults for nearly 20 years suggests a “synergistic” link between exercise and good vitamin D levels in reducing the risk of heart attacks and strokes.
Both exercise and adequate vitamin D have long been implicated in reducing heart disease risks, but in a new study — one not designed to show cause and effect — the researchers investigated the relationship between these two health factors and their joint role in heart health. Their findings, which were published in the April 1 issue of The Journal of Clinical Endocrinology & Metabolism, identified a positive and direct relationship between exercise and vitamin D levels in the blood, which may provide evidence that exercise may boost vitamin D stores. They also found that the two factors working together seemed to somehow do more than either factor alone to protect the cardiovascular system. The researchers caution that their study is an observational one and that long-term, carefully controlled clinical trials would be needed to establish evidence for cause and effect. Nevertheless, the study does support the notion that exposure to the “sunshine” vitamin D and exercise are indicators of good health.
“In our study, both failure to meet the recommended physical activity levels and having vitamin D deficiency were very common” says Erin Michos, M.D., M.H.S., associate director of preventive cardiology and associate professor of medicine at the Ciccarone Center for the Prevention of Heart Disease at the Johns Hopkins University School of Medicine. “The bottom line is we need to encourage people to move more in the name of heart health.” Michos adds that exposure to a few minutes a day of sunlight in non-winter seasons, eating a well-balanced meal that includes oily fish such as salmon, along with fortified foods like cereal and milk, may be enough to provide adequate levels of vitamin D for most adults.
For their data analysis, the Johns Hopkins researchers used previously gathered information from the federally funded Atherosclerosis Risk in Communities study beginning in 1987 and collected from 10,342 participants initially free of heart or vascular disease. Information about participants was updated and followed until 2013, and included adults from Forsyth County, North Carolina; Jackson, Mississippi; greater Minneapolis, Minnesota; and Washington County, Maryland. The participants were an average age of 54 at the start of the study and 57 percent were women. Twenty-one percent were African-American, with the remaining participants identifying as white.
In the first visit between 1987 and 1989, participants self-reported their exercise levels, which were compared to the American Heart Association recommendations of more than 150 minutes per week of moderate intensity exercise or 75 minutes per week or more of vigorous intensity. The researchers used the information to classify each participant’s exercise level as adequate, intermediate or poor. People with adequate exercise levels met the AHA’s recommendations, those with intermediate levels exercised vigorously for up to 74 minutes per week or exercised moderately for less than 149 minutes a week, and those classified as poor didn’t exercise at all. About 60 percent of the participants had inadequate exercise in the poor or intermediate categories. The researchers converted the exercise to metabolic equivalent tasks (METs), an exercise intensity scale used by cardiologists and other clinicians to assess fitness. They then calculated physical activity levels by multiplying METs by minutes per week of exercise.
Reviewing data from the second study visit by each participant between 1990 and 1992, the researchers measured vitamin D levels in the blood by detecting the amount of 25-hydroxyvitamin D. Anyone with less than 20 nanograms per milliliter of 25-hydroxyvitamin D was considered deficient for vitamin D, and levels above 20 nanograms per milliliter were considered adequate. Thirty percent of participants had inadequate vitamin D levels.
In the first part of their study, the Johns Hopkins team showed that exercise levels positively corresponded to vitamin D levels in a direct relationship, meaning that the more one exercised, the higher their vitamin D levels seemed. For example, people with adequate exercise had an average 25-hydroxyvitamin D level of 26.6 nanograms per milliliter, those with intermediate exercise had 24.4 nanograms per milliliter, and those with poor exercise had 22.7 nanograms per milliliter. Those meeting recommended levels of exercise at visit 1 had a 31 percent lower risk of being vitamin D deficient at visit 2. Yet, the researchers only saw such a positive relationship between exercise and vitamin D in whites and not African-Americans.
In the next part of the study, they found that the most active participants with the highest vitamin D levels had the lowest risk for future cardiovascular disease. Over the 19 years of the study, 1800 adverse cardiac events occurred, including heart attack, stroke or death due to heart disease or stroke. After adjusting the data for age, sex, race, education, smoking, alcohol use, blood pressure, diabetes, high blood pressure medication, cholesterol levels, statin use and body mass index, the researchers found that those people who met both the recommended activity levels and had vitamin D levels above 20 nanograms per milliliter experienced about a 23 percent less chance of having an adverse cardiovascular event than those people with poor physical activity who were deficient for vitamin D. On the other hand, people who had adequate exercise but were vitamin D deficient didn’t have a reduced risk of an adverse event. In other words, the combined benefit of having adequate vitamin D and exercise levels was better than either health factor alone.
But Michos says that sun exposure may not be the whole story of the direct relationship found between exercise and vitamin D levels, since vitamin D produced by the skin after exposure to sunlight tends to level off when the body makes enough, and the levels in these participants didn’t show signs of doing so. She says this points to evidence that there may be something else going on in the body that causes vitamin D and exercise to positively influence levels of each other. For example, people who exercise may also have other healthy habits that influence vitamin D levels such as lower body fat and a healthier diet. Alternatively, people who exercise may take more vitamin supplements.
As for the racial disparity they saw, this could mean promoting physical activity may not be as effective for raising vitamin D levels in African-Americans as in whites. Michos notes that people with darker skin produce vitamin D less efficiently after sun exposure, possibly due to the greater amount of melanin pigment, which acts as a natural sunscreen. African-Americans also tend to have lower levels of 25-hydroxyvitamin D overall but they don’t seem to experience the same consequences, such as bone fractures, that whites have with similarly low levels.
Michos cautions that people who meet the recommended daily amount of 600 to 800 International Units a day and who have adequate levels of vitamin D don’t need to take additional vitamin supplements. “More isn’t necessarily better once your blood levels are above 20 nanograms per milliliter,” says Michos. “People at risk of bone diseases, have seasonal depression, or are obese should have their physicians measure vitamin D levels to ensure they’re adequate, but for many, the best way to ensure adequate blood levels of the vitamin is from sun exposure, healthy diet, being active and maintaining a normal body weight.” She adds, “Just 15 minutes of sunlight in the summer produces about 3000 international units of vitamin D depending on latitude and skin pigmentation, which is equivalent to 30 glasses of milk. Just be sure to use sunscreen if you plan to be outside longer than 15 minutes.”
While the health boost from regular physical activity is undisputed, the benefits of vitamin D supplements haven’t yet been proven for heart health. Michos notes that a recent randomized clinical trial published in JAMA Cardiology failed to show any cardiovascular benefit with high-doses of monthly vitamin D supplements among participants living in New Zealand. She says that larger studies including more diverse populations of patients and different dosing regimens are currently on-going and, when published, will provide further insight and guide recommendations for patients.
Additional authors of the study included Kathleen Chin, Di Zhao, Martin Tibuakuu, Seth Martin, Chiadi Ndumele, Roberta Florido and Eliseo Guallar of The Johns Hopkins University; Gwen Windham of the University of Mississippi Medical Center; and Pamela Lutsey of the University of Minnesota.
The study was funded by grants from the National Institute of Neurological Disorders and Stroke (R01 NS072243), the National Heart, Lung, and Blood Institute (R01 HL103706 and R01 HL103706-S1), and the Blumenthal Scholars Fund. The ARIC study was funded by contracts from the NHLBI (HHSN268201100007C, HHSN268201100008C, HHSN268201100009C, HHSN268201100010C, HHSN268201100011C and HHSN268201100012C).
Martin receives research funding from the Aetna Foundation and Google and consulted for Abbott Nutrition, Pressed Juicery and Quest Diagnostics. He holds a patent for a new way of measuring cholesterol. Michos has participated in a Siemens Healthcare Diagnostics trial.
Newswise —
The U.S. Preventive Services Task Force issued recommendations earlier this month that change its stance on prostate screenings, suggesting that men have conversations about it with their doctors.
The task force, made up mostly of primary care and family physicians, uses evidence to provide grading assessments for different types of screening modalities.
Since 2012, the group has said there is no need for men to have a blood test that screens the level of PSA – prostate-specific antigen – in the blood.
“The rationale was that we were picking up cancers of the prostate that were insignificant – ones you would die with rather than from – and possibly treating people unnecessarily,” said Dr. Jay Raman, chief of the Division of Urology at Penn State Health Milton S. Hershey Medical Center.
Now, the task force recognizes that such a blanket statement for all ages may keep men for whom the disease is curable from catching it at the early stages.
“When people began looking at statewide and national statistics, they started finding greater reported rates of metastasis – the disease spreading outside the prostate,” Raman said. “Once that happens, it’s more likely you could end up dying of your cancer.”
The new guidelines recommend that men aged 55 to 69 with no signs of prostate cancer have a conversation with their doctor about the benefits and drawbacks of screening for the disease.
The screening typically involves two parts – a blood test to determine the level of PSA in the body, and a rectal examination to feel for lumps, bumps or abnormalities.
“Neither is perfect, but they complement each other,” Raman said. “Part of the challenge for clinicians is to figure out if the combination of the exam and PSA results is concerning enough to go down the road to investigate for cancer.”
Because the prostate gets bigger as a man ages, the amount of PSA in the blood that is considered normal increases with age. For instance, a PSA of 5 may not be an issue for a 70-year-old, but it may be for a 55-year-old.
The task force still recommends against the screenings for men age 70 and older, although other organizations such as the American Urological Association suggest screening discussions in this age cohort if the person has an anticipated life expectancy of more than 10 years.
“This provides some standardized guidelines in a reasonable and measured manner,” Raman said. “Rather than not screening anyone, we should determine who the people are that need screening, diagnose and potentially treat those who need it, and monitor those whose cancers can be safely followed.”
Raman is also pleased that the new draft recommendations have been opened up for feedback from urologists and others who treat prostate cancer.
“One big criticism of the 2012 recommendation was that it was crafted almost exclusively by physicians who do not treat prostate cancer,” he said. “The current USPSTF statement appropriately includes some prostate cancer specialists which creates a reasonable balance for the panel.”
The Medical Minute is a weekly health news feature produced by Penn State Health Milton S. Hershey Medical Center. Articles feature the expertise of faculty physicians and staff, and are designed to offer timely, relevant health information of interest to a broad audience.
Newswise — Chicago –
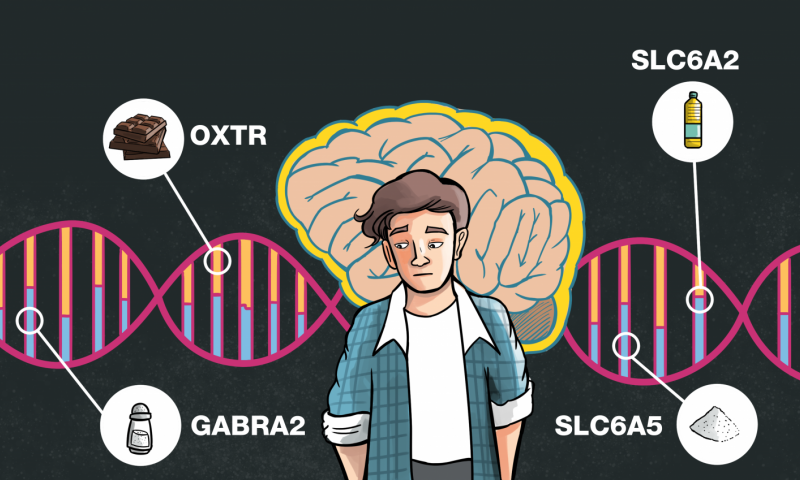
Have you ever wondered why you keep eating certain foods, even if you know they are not good for you? Gene variants that affect the way our brain works may be the reason, according to a new study. The new research could lead to new strategies to empower people to enjoy and stick to their optimal diets.
Silvia Berciano, a predoctoral fellow at the Universidad Autonoma de Madrid, will present the new findings at the American Society for Nutrition Scientific Sessions and annual meeting during the Experimental Biology 2017 meeting, to be held April 22–26 in Chicago.
“Most people have a hard time modifying their dietary habits, even if they know it is in their best interest,” said Berciano. “This is because our food preferences and ability to work toward goals or follow plans affect what we eat and our ability to stick with diet changes. Ours is the first study describing how brain genes affect food intake and dietary preferences in a group of healthy people.”
Although previous research has identified genes involved with behaviors seen in eating disorders such as anorexia or bulimia, little is known about how natural variation in these genes could affect eating behaviors in healthy people. Gene variation is a result of subtle DNA differences among individuals that make each person unique.
For the new study, the researchers analyzed the genetics of 818 men and women of European ancestry and gathered information about their diet using a questionnaire. The researchers found that the genes they studied did play a significant role in a person’s food choices and dietary habits. For example, higher chocolate intake and a larger waist size was associated with certain forms of the oxytocin receptor gene, and an obesity-associated gene played a role in vegetable and fiber intake. They also observed that certain genes were involved in salt and fat intake.
The new findings could be used to inform precision-medicine approaches that help minimize a person’s risk for common diseases—such as diabetes, cardiovascular disease and cancer—by tailoring diet-based prevention and therapy to the specific needs of an individual.
“The knowledge gained through our study will pave the way to better understanding of eating behavior and facilitate the design of personalized dietary advice that will be more amenable to the individual, resulting in better compliance and more successful outcomes,” said Berciano.
The researchers plan to perform similar investigations in other groups of people with different characteristics and ethnicities to better understand the applicability and potential impact of these findings. They also want to investigate whether the identified genetic variants associated with food intake are linked to increased risks for disease or health problems.
Silvia Berciano will present this research at 5–7 p.m. Saturday, April 22, in Hall F Swing Space, McCormick Place Convention Center (poster D151 996.2) and during the Nutrigenomics and Personalized Nutrition Session at 10:30-12:30 p.m. Monday, April 24, in Center Room S103BC (abstract). Contact the media team for more information or to obtain a free press pass to attend the meeting.
Image available.
About Experimental Biology 2017
Experimental Biology is an annual meeting comprised of more than 14,000 scientists and exhibitors from six host societies and multiple guest societies. With a mission to share the newest scientific concepts and research findings shaping clinical advances, the meeting offers an unparalleled opportunity for exchange among scientists from across the United States and the world who represent dozens of scientific areas, from laboratory to translational to clinical research. www.experimentalbiology.org #expbio
About the American Society for Nutrition (ASN)
ASN is the preeminent professional organization for nutrition research scientists and clinicians around the world. Founded in 1928, the society brings together the top nutrition researchers, medical practitioners, policy makers and industry leaders to advance our knowledge and application of nutrition. ASN publishes three peer-reviewed journals and provides education and professional development opportunities to advance nutrition research, practice and education.
www.nutrition.org
Find more news briefs and tipsheets at: https://www.eurekalert.org/meetings/eb/2017/newsroom.
###
SEE ORIGINAL STUDY
Newswise — Chicago –
A new study finds that carvedilol, a drug typically used to treat high blood pressure, can protect against the sun-induced cell damage that leads to skin cancer. Researchers serendipitously discovered the beta blocker’s cancer-fighting properties after making an error in the lab.
Sherry Liang, a graduate student at the Western University of Health Sciences College of Pharmacy, will present the new findings at the American Society for Pharmacology and Experimental Therapeutics annual meeting during the Experimental Biology 2017 meeting, to be held April 22-26 in Chicago.
“What began as an experimental error led to a very interesting scientific discovery,” said Ying Huang, PhD, coleader of the research team with Bradley T. Andresen, PhD. “Our research could lead to the development of a class of new cancer-preventive agents.”
Carvedilol’s cancer-fighting properties were discovered when a former graduate student in Huang’s lab was studying whether carvedilol and similar beta blockers might increase cancer risk. The student inadvertently tested carvedilol’s anticancer effect rather than its ability to promote cancer, finding that carvedilol surprisingly showed some protective effects against skin cancer.
The researchers then conducted experiments with cell cultures and mice to see if carvedilol could prevent skin cancer caused by ultraviolet-B (UVB), the portion of sunlight that tends to damage the skin's top epidermal layers and plays a key role in skin cancer development.
The researchers found that carvedilol exhibited a protective effect in cultured mouse skin cells exposed to UVB and in hairless mice given the drug after UVB exposure. The experiments showed that carvedilol acted by protecting cells against the cancer-causing DNA damage and cell death produced by UVB. Hairless mice exposed to UVB and given carvedilol showed decreases in both the severity and number of tumors that developed compared to those not given carvedilol. The mouse studies also showed that carvedilol delayed skin tumor formation more than sunscreen.
The researchers also discovered that not all beta blockers show cancer preventive properties, indicating that the cancer-fighting beta blockers likely act on not yet identified molecules. “We have preliminary data indicating that the cellular targets for carvedilol are not related to the beta-adrenergic receptors that are the commonly accepted targets for all beta blockers,” said Andresen. “They likely target unexpected mechanisms involved in cancer development.”
The researchers aim to incorporate carvedilol or similar beta blockers into a skin cream or spray that could hopefully be used to prevent skin cancer arising from UV light exposure. The treatment would act on the skin without affecting blood pressure and heart rate, which are commonly altered by beta blockers. Understanding carvedilol’s mechanisms of action could also allow scientists to design completely new treatments that target these mechanisms without introducing any cardiovascular effects.
Sherry Liang will present the findings at 12:30–2:30 p.m. Tuesday, April 25, in Hall F, McCormick Place Convention Center (poster D151 996.2) (abstract). Another poster from the same group will be presented at 12:30–2:30 p.m. Sunday, April 23, in Hall F, McCormick Place Convention Center (poster D146 671.13) (abstract). Contact the media team for more information or to obtain a free press pass to attend the meeting.
Video available.
About Experimental Biology 2017
Experimental Biology is an annual meeting comprised of more than 14,000 scientists and exhibitors from six host societies and multiple guest societies. With a mission to share the newest scientific concepts and research findings shaping clinical advances, the meeting offers an unparalleled opportunity for exchange among scientists from across the United States and the world who represent dozens of scientific areas, from laboratory to translational to clinical research.
www.experimentalbiology.org #expbio
About the American Society for Pharmacology and Experimental Therapeutics (ASPET)
ASPET is a 5,100 member scientific society whose members conduct basic and clinical pharmacological research within the academic, industrial and government sectors. Our members discover and develop new medicines and therapeutic agents that fight existing and emerging diseases, as well as increase our knowledge regarding how therapeutics affects humans. www.aspet.org
Find more news briefs and tipsheets at: https://www.eurekalert.org/meetings/eb/2017/newsroom
###
SEE ORIGINAL STUDY