News
Newswise —
A common cause of hair loss and breakage known as acquired trichorrhexis nodosa, or TN --often more prevalent in African-Americans -- can actually be remedied through appropriate use of cleansing products, hair care and styling practices, say researchers at Johns Hopkins.
"It's imperative that we offer dermatologist and patients alike easy tips for resolving TN, one of the few forms of hair loss that can be resolved fairly quickly with nonmedical options," says Crystal Aguh, M.D., assistant professor of dermatology at the Johns Hopkins University School of Medicine and co-author of Fundamentals of Ethnic Hair: The Dermatologist's Perspective. "Our recommendations are acceptable for those of all ethnic backgrounds experiencing hair breakage, and dermatologists should feel comfortable discussing these techniques with every patient seen."
In a literature review published ahead of print in the Journal of Dermatological Treatment, the investigators outline risk factors and simple recommendations for dermatologists, who are often uncomfortable with advising patients, especially those of color, on appropriate practices necessary for avoiding hair loss and breakage.
In the report, researchers analyzed the risk factors for TN. They found that thermal styling tools, such as the use of flat irons and blow dryers, as well as chemical processing, such as permanent dye and straightening, tend to damage the protective outer layer of the hair shaft, called the cuticle. This can alter the hair's protein structure, which causes the cortical fibers to be exposed and fray, leading to weak points where breakage occurs.
Patients of African heritage (African-American and Afro-Caribbean) who tend to have tightly coiled hair are at increased risk for hair loss and damage from TN. This is because there are structural differences within the hair shaft -- African hair fibers have an asymmetric shape and curvature, resulting in points of geometric weakness in the hair shaft. Curly hair also has differences in hydration properties, causing it to be drier and more susceptible to breakage.
Cleansing is the cornerstone of any health hair regimen, says Aguh. Inadequate cleansing of the hair and scalp can result in the buildup of product residue, leading to problems such as seborrheic and irritant dermatitis.
As part of the literature review, investigators also describe simple over-the-counter, nonmedical remedies that can be recommended by dermatologists when treating patients with TN. First, choosing the appropriate shampoo based on hair types, the researchers say, is incredibly important when trying to reduce breakage and loss. Most shampoos include surfactants, which are the active ingredients that bind sebum and water. There are three types of surfactants to look for when selecting a shampoo -- anionic, amphoteric and nonionic. Anionic surfactants tend to be best suited for those with oily hair and are very effective at cleansing the hair, but this can leave the hair feeling dry and prone to breakage. Nonionic or amphoteric surfactants are recommended for those with natural black hair or dry, damaged or color-treated hair. These types of shampoos are gentler and less likely to strip the hair of moisture.
Second, the frequency at which the hair is cleansed is key in minimizing the impact of TN. Frequency varies greatly based on many factors, such as age, ethnic origin and condition of the hair. Those with tightly curled hair types should shampoo their hair less frequently, since sebum has a harder time coating this particular type of hair strand. Patients with straight hair should shampoo more frequently because sebum coats the entire strand, leading to oily hair.
"Patients with dry, damaged or tightly curled hair should limit their shampooing to no more than once per week. Those with straight hair, however, can shampoo daily," recommends Aguh.
Third, conditioning the hair is arguably one of the most important steps for a healthy hair regimen, say the investigators. Conditioners increase hair manageability, help eliminate static electricity and can temporarily mend hair shaft damages. They come in many different formulations depending on the desired effect -- rinse-out, deep, leave-in and protein-containing. Rinse-out conditioners are applied immediately after the use of shampoo and rinsed out with water. While rinse-out conditioners increase manageability and add shine, they're less effective in repairing hair damage due to their short contact time with the hair. Unlike rinse-out, deep conditioners are left on the hair for at least 10 minutes and include the use of heat. Since they are usually formulated as deep creams, they enhance moisture in the hair. Deep conditioners are beneficial for severely damaged hair. Leave-in conditioners are put in the hair after shampooing and conditioning, and are not rinsed out. Leave-ins can be applied daily and are ideal for preventing damage from everyday grooming. The most beneficial conditioning treatment for those with dry and damaged hair is protein-containing conditioners. These can be formulated as rinse-out, deep or leave-in. Though protein-containing treatments help with breakage, it is recommend to only apply on a monthly or bimonthly basis, since overuse can lead to brittleness.
Lastly, another way to help minimize hair breakage and prevent or treat TN is to try the repurposed soak-and-smear method for hair care. This method increases moisture retention, which in return enhances hair elasticity and reduces tangles. It forms increased protection from damage. The repurposed soak-and-smear method for hair care is as follows:
1. Shampoo and/or condition the hair normally and lightly blot hair with a towel.2. Follow with the application of a water-based leave-in conditioner to the hair.3. Immediately apply an oil or thick, occlusive moisturizer, such as coconut oil, olive oil, jojoba oil, petrolatum or mineral oil, to the hair.4. Allow the hair to air dry and style as desired.
This method can be completed as often as needed throughout the week and modified depending on shampoo/conditioning needs. The repurposed soak and smear is especially beneficial for patients with tightly coiled hair, as it helps reduce dryness associated with overprocessing from heat and chemical applications.
These recommendations can greatly improve the hair condition of those with TN. Since hair is a nonliving tissue, total repair of the hair shaft is not possible. Implementation of proper cleansing and conditioning techniques, as well as proper product selection, improve the overall health of hair, making it more resilient to trauma. "Patients need to be advised on how to improve the quality of their cleansing and conditioning routines," says Aguh. "These are the foundation of a healthy hair routine."
Additional authors of this study include Shawn G. Kwatra of the Johns Hopkins University School of Medicine and Alessandra Haskin of Howard University College of Medicine.
Newswise — FAYETTEVILLE, Ark. –
A team of biomedical engineering researchers at the University of Arkansas have identified a cause of fluid swelling of the brain, or cellular edema, that occurs during a concussion.
The researchers discovered that pre-treating the cells with an existing, FDA-approved drug used for epilepsy and altitude sickness reduces the expression of a specific protein that causes swelling.
Their findings were published in a recent issue of Nature’s Scientific Reports.
“Our study found that mild traumatic brain injury resulted in increased expression of a protein called aquaporin-4, which caused a massive cellular influx of fluid, leading to increased astrocyte cell volume and injury,” said Kartik Balachandran, assistant professor of biomedical engineering. “We then worked with a drug called Acetazolamide. Our results showed that Acetazolamide minimized cell swelling and injury, suggesting a therapeutic role for this drug in reducing the detrimental effects of concussions.”
In addition to Balachandran, who led the study, the research was conducted by Nasya Sturdivant, biomedical-engineering doctoral candidate; Jeffrey Wolchok, assistant professor of biomedical engineering; and partners at the FDA’s National Center for Toxicological Research in Jefferson, Arkansas.
Mild traumatic brain injury, also known as a concussion, is a devastating condition that is commonly experienced in car accidents, full-contact sports and battlefield injuries. One of the main factors that leads to the high death rate in patients who experience mild traumatic brain injury is the swelling or edema of astrocytes, the most abundant cell type in the brain.
The researchers engineered a benchtop bioreactor to examine astrocyte cells. This device helped them see that mild traumatic brain injury led to an increased expression of aquaporin-4, the protein that causes a large cellular influx of fluid, which in turn leads to increased astrocyte cell volume.
“This study demonstrates the collaborative neuro-engineering efforts that are contributing to both diagnostic and therapeutic methods for addressing traumatic brain injury,” said Raj Rao, professor and chair of the Department of Biomedical Engineering at the University of Arkansas.
The research was funded by the National Science Foundation.
-30-
CONTACTS: Kartik Balachandran, assistant professor, biomedical engineeringCollege of Engineering479-575-3376, kbalacha@uark.edu
Matt McGowan, science and research communications officerUniversity Relations479-575-4246, dmcgowa@uark.edu
SEE ORIGINAL STUDY
Loyola Medicine
Julia Conkin suffered a childhood bout with the flu that triggered progressive hearing loss. Matt Kircher, MD, an ear, nose and throat surgeon at Loyola, implanted a cochlear implant in a one-hour outpatient surgery. She now is able to hear conversations and listen to music without the use of a hearing aid.
Source Newsroom: Loyola University Health System
Newswise — MAYWOOD, IL – Due to a childhood bout with the flu, Julia Conkin suffered progressive hearing loss that started in her left ear and continued to her right ear.
”I couldn’t hear conversations or even listen to music without the use of a hearing aid, and due to my worsening condition, hearing aids weren’t even working well," Ms. Conkin said.
Ms. Conkin consulted with the multidisciplinary otolaryngology and audiology team at Loyola Medicine.“Julia’s hearing was so bad she had to rely on sign language and that severely limited the number of people she could communicate with,” said Loyola audiologist Adriana Russ, AuD. “She came to Loyola to see if she was a candidate for a cochlear implant.”
Matt Kircher, MD, an ear, nose and throat surgeon, implanted a cochlear implant in a one-hour outpatient surgery. “Julia had suffered from really bad hearing for a very long time and was at the end of her rope and looking for the next step,” said Dr. Kircher. "A cochlear implant is a device usually used in patients like Julia who have failed hearing aids.”
Unlike a traditional hearing aid, a cochlear implant does not make sound louder or clearer; rather it bypasses the damaged parts of the auditory system and stimulates the hearing nerve, allowing sound to be received.
The cochlear implant system contains two parts: the external processor and the internal implant. The external processor is worn behind the ear and includes a speech processor, a microphone and a battery compartment. The internal implant is surgically placed under the skin behind the ear. These two parts work together to allow for the perception of sound.
Dr. Kircher has performed hundreds of cochlear implants. He makes a small incision behind the ear, exposing the cochlea. Then, an opening is made in the cochlea and the electrodes for the implant are inserted. The internal implant is then placed beneath the skin.
A few weeks after implantation, Dr. Kircher and the team place the external processor, microphone and implant transmitter. A Loyola audiologist activates the implant. “With Julia, the expectations for hearing improvement were modest but the results were spectacular,” said Russ.
Ms. Conkin calls her cochlear implant a life-changer. "I noticed almost immediately after my implant was activated that I could hear things I had not heard for years, like music and conversations at gatherings,” she said. “It was beautiful to hear other people.”
Loyola Medicine is nationally recognized for its expertise in diagnosing and treating a broad range of ear, nose and throat conditions and providing integrated services for optimal patient care.
Newswise —
Conventional, high-dose chemotherapy treatments can cause the fibroblast cells surrounding tumors to secrete proteins that promote the tumors’ recurrence in more aggressive forms, researchers at Taipei Medical University and the National Institute of Cancer Research in Taiwan and University of California, San Francisco, have discovered. Frequent, low-dose chemotherapy regimens avoid this effect and may therefore be more effective at treating certain types of breast and pancreatic cancer, according to the murine study “Metronomic chemotherapy prevents therapy-induced stromal activation and induction of tumor-initiating cells,” which will be published online November 23 in The Journal of Experimental Medicine.
Chemotherapy drugs are usually administered to cancer patients every few weeks at a high “maximum tolerated” dose. Though this approach kills the majority of tumor cells, it often spares a small number of tumor-initiating cells (TICs) that subsequently give rise to new tumors. Moreover, these recurring tumors are often more aggressive and able to metastasize to other tissues, in part because high doses of chemotherapy drugs also affect cells in the stromal tissue that surrounds tumors, including immune cells and blood vessel endothelial cells.
Kelvin Tsai at Taipei Medical University and Valerie Weaver at the University of California, San Francisco, decided to investigate the effect of chemotherapy on fibroblasts, a major component of the stroma in desmoplastic tumors such as breast cancer and pancreatic ductal adenocarcinoma.
The researchers found that, in response to the maximum tolerated doses of several commonly used chemotherapy drugs, breast cancer–associated fibroblasts secrete large amounts of cell signaling proteins called ELR+ chemokines. These proteins promoted tumor growth and metastasis in mice by converting neighboring cancer cells into TICs, stimulating the formation of blood vessels within the tumor and enhancing the recruitment of immune cells called macrophages.
Recent studies have suggested that treating patients with low doses of chemotherapy drugs at more frequent, even daily, intervals may be more effective than traditional chemotherapeutic approaches. Tsai and colleagues found that such “low-dose metronomic” regimens did not induce the production of ELR+ chemokines by cancer-associated fibroblasts. This, in turn, reduced the fibroblasts’ ability to promote TIC formation, blood vessel growth, and macrophage recruitment.
Mice with breast cancer or pancreatic ductal adenocarcinoma therefore responded better to low-dose metronomic chemotherapy, surviving longer than mice treated with the maximum tolerated dose. “Our results lend support to the emerging paradigm that stroma-derived signals contribute to tumor pathology,” Tsai says. “They also suggest that low-dose metronomic chemotherapy or targeting the chemokine signaling mediated by chemo-treated fibroblasts may improve the therapeutic outcome in desmoplastic cancers.”
Chan et al. 2016. J. Exp. Med. https://doi.org/10.1084/jem.20151665
# # #
Newswise — ANN ARBOR, Mich. –
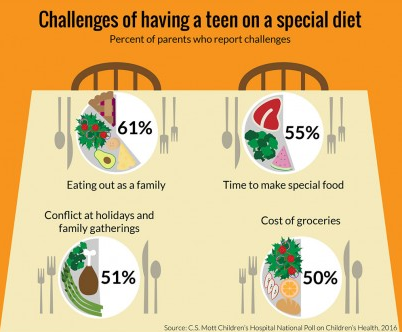
Planning a holiday meal can be hectic, and some families will be managing an extra stressor: accommodating the dietary restrictions of teens on gluten-free, vegan or other special diets.
For a variety of reasons, many teens choose diets that go beyond cutting calories and reducing portion sizes – instead, these special diets restrict entire food groups. That could mean added costs and new logistical challenges for families, suggests a new national poll.
One in six parents say their teen has tried a diet that is vegetarian (9 percent), gluten-free (6 percent), vegan (4 percent) or paleo (2 percent) at some point in the past two years, according to the C.S. Mott Children’s Hospital National Poll on Children’s Health at the University of Michigan.
The diet changes weren’t always harmonious. Roughly half of parents in the Mott poll said the special diets caused conflicts at holiday and family gatherings.
“Teen diets that limit food options can impact the whole family,” says poll co-director Sarah Clark, M.P.H. “That can lead to conflict at the holidays if the diet doesn’t include the mainstays of the family’s traditional meal, and the teen refuses to eat Granny’s famous mac & cheese, or the turkey Aunt Emma spent all day preparing.”
Other difficulties are everyday challenges, like finding a suitable place for the whole family to dine out (61 percent), extra time spent preparing diet-friendly food (55 percent), the stress of family members eating different meals (54 percent) and the added expense of buying special diet foods (50 percent).
“Parents can work with teens to minimize any burden on family members, such as asking the teen to prepare his or her own meals, or finding diet-compliant versions of the family’s favorite foods,” says Clark.
Too little health advice?
Parents gave a variety of reasons for why their teen tried the special diet: 32 percent said it was health-related, while 29 percent said it was because another family member was on the same diet. Other motives included a friend’s suggestion (17 percent) and the diet’s environmental impact (14 percent).
More than half of parents say they did their homework when their teen started a special diet — with nearly half suggesting that their teen began taking vitamins or supplements in tandem. Just 17 percent brought their teen to a health care provider to discuss whether the diet was healthy.
“Parents may not recognize this as a situation that would benefit from advice from a health care professional,” says Clark.
About half of parents (52 percent) think the special diet had a positive impact in their teen feeling healthier, while 41 percent believe it made no difference.
On the other hand, 7 percent say the diet negatively impacted their teen’s health.
“There are situations where diets that restrict certain food groups can result in teens not getting enough protein, iron, calcium or other essential parts of a healthy diet,” said Clark. “Advice from a dietician or nutritionist can help families weigh the risks and benefits to determine practical options for teens looking for a healthier lifestyle.”
The Mott Poll report was based on responses from a nationally-representative group of 910 parents who had at least one child between the ages of 13 and 18.
Newswise — ANN ARBOR, Mich. --
Young adults have access to an outpatient procedure that can stop progressive vision loss.
Corneal cross-linking strengthens the cornea if it’s been weakened by keratoconus, other corneal disease or, rarely, as a complication of LASIK surgery.
What’s new and exciting, says cornea specialist Shahzad I. Mian, M.D., is the option to prevent vision loss before patients with keratoconus need corrective lens and, even more significantly, to reduce the need for corneal transplants.
Keratoconus tends to be diagnosed among teens and young adults and progresses for 10 to 20 years before slowing. The earlier it can be treated, the better the outcome.
“Up to now, treatments have been focused on management of symptoms, often with specialized contact lens and, if patients don’t see better, then corneal transplants,” Mian says. “We can now offer a treatment that, if provided early in the disease, can help maintain better vision.”What to expect from corneal cross-linking
Keratoconus causes the cornea — the front window of the eye — to be distorted and shaped like a cone.
The abnormal shape can cause vision changes, such as light sensitivity, glare and irritation, and can lead to frequent changes in glasses and contact lens prescriptions for nearsightedness.
The cornea contains tiny fibers of protein called collagen, and these fibers help hold the cornea in place and keep it from distorting.
Corneal cross-linking involves removing the front layer of the cornea and administering an eye drop of liquid riboflavin (vitamin B12) to the surface of the eye. Ultraviolent light is then delivered to the eye at differing levels of time and intensity. The eye drop helps the cornea absorb the ultraviolet light and stiffen.
The procedure lasts 60 to 90 minutes. Patients will see results after six months to one year.
Newswise — SAN DIEGO –
A new study in rats could begin to explain why allergies during pregnancy are linked to higher risks for attention-deficit hyperactivity disorder and autism in children.
Researchers at The Ohio State University found significant changes in the brain makeup of fetuses and newborn rats exposed to allergens during pregnancy.
Animals that lived to adulthood after allergen exposure before birth showed signs of hyperactivity and antisocial behavior and decreased anxiety, found a research team led by Kathryn Lenz, an Ohio State assistant professor of psychology.
“This is evidence that prenatal exposure to allergens alters brain development and function and that could be an underappreciated factor in the development of neurodevelopmental disorders,” said Lenz, who presented her research Nov. 16 in San Diego at Neuroscience 2016, the annual meeting of the Society for Neuroscience.
Though there are established links between allergies and ADHD and autism – as well as between inflammation and risk of autism, schizophrenia and ADHD – the cellular-level changes that could contribute to those connections largely remain a mystery.
Autism and ADHD are both three to four times as common in boys than in girls, Lenz said. And so she and her collaborators set out to look for sex differences in the rats as well.
“We’re really interested in figuring out unknown factors in psychological disorders and in differences between male and female brain development as it relates to autism, ADHD and other disorders,” Lenz said.
To study the effects of allergies on offspring, researchers sensitized female rats to ovalbumin (found in egg whites) before pregnancy. Then, 15 days into their pregnancies, they exposed them to the allergen, prompting an immune response in the animals.
They analyzed whether prenatal allergen exposure changed the number and behavior of immune cells in the developing brain of offspring. They explored possible changes in young rats’ physical activity, anxiety-like behavior, ability to learn and sociability. And they examined the density of dendritic spines in the juvenile animals’ brains. The spines protrude from neurons and are vital to cellular-level communication in the brain.
Rats exposed to allergens before birth had higher levels of immune cells called mast cells in the brain and lower numbers of immune cells called microglia, regardless of the animals’ gender.
Animals with allergic mothers were hyperactive, but had lower levels of anxiety-like behavior. When they interacted with other juvenile rats, the males in the allergen group were less likely to roughhouse with their peers.
“Young rats engage in social play and males are more rough and tumble and usually play much more than females,” Lenz said.
“The males born to the allergen-exposed mothers looked more like females. They were more socially reserved. They were really hyperactive, but socially disengaged. That looks a bit like ADHD.”
And when the researchers looked at the animals’ ability to be mentally flexible, the rats born to allergic mothers had a tougher time, Lenz said.
“They have to use rules to find a reward – a Cheerio in a terracotta pot – and the rules we give them keep shifting,” Lenz said, explaining that in one test the treat might be in a pot covered in sandpaper and in another test it might be in a pot covered in velvet.
The rats in the allergen group weren’t as capable of adapting to the changing parameters of the test, and the males had deficits that were more significant than the females.
Early data from the study shows that the dendritic spines – the points of synaptic connection between cells in the frontal cortex of the animals’ brains – were decreased in males with allergy exposure and increased in their female counterparts.
The study was supported by The National Institute of Mental Health.
Lenz’s collaborators at Ohio State were undergraduate students Annemarie Krug and Aarohi Joshi and laboratory technician Anabel Galan.
#
Newswise — WINSTON-SALEM, N.C. –
What’s the best way to stop type 2 diabetes?
Find it before it becomes a problem.
“The phrase I use is prevention by detection,” said Joseph Aloi, M.D., section chief of endocrinology and metabolism at Wake Forest Baptist Medical Center in Winston-Salem, North Carolina.
It’s no secret that diabetes – elevated blood glucose levels caused by the body’s failure to produce enough insulin (type 1) or properly use it (type 2) to process sugars – has reached epidemic proportions in the United States. According to the federal Centers for Disease Control and Prevention (CDC), approximately 29 million people in this country have diabetes, with type 2, formerly known as adult-onset diabetes, accounting for more than 90 percent of those cases. If left unchecked, diabetes can lead to serious complications, including heart disease, kidney failure, stroke, blindness and the loss of toes, feet and legs.
What’s less known is that nearly three times as many Americans – roughly 86 million – have prediabetes, a condition where blood sugar levels are above normal but still below the threshold for type 2. Prediabetes generally doesn’t produce noticeable symptoms, so the vast majority of people with the condition – nine out of 10, according to the CDC – don’t even know they have it.
But the progression from prediabetes to type 2 is not inevitable, and there’s a common blood test called the A1C that can determine whether a person’s blood glucose levels require attention.
“Prediabetes is a great opportunity to prevent diabetes,” Aloi said. “The A1C test really helps you hone in on whether there’s a problem, and if there is, to start addressing it. It’s a simple, inexpensive test that doesn’t require any special preparation but can provide a lot of good information.”
Formally the glycated hemoglobin test, the A1C measures the percentage of glycosylated hemoglobin – think sugar-coated red blood cells – in the bloodstream, which indicates a person’s average blood glucose level over the previous three months. The A1C provides a more accurate assessment than a fasting plasma glucose test, which uses a blood sample taken from a person who has abstained from food and drink for at least eight hours.
“The fasting test is a snapshot of what your blood sugar level is at that one specific time, which may or may not be representative of what’s really going on,” Aloi said. “The A1C test, on the other hand, is sort of a report card for the past 90 days, and that’s a more valuable indicator.”
So who should get tested?
Various institutions and organizations offer different recommendations but generally agree that you should at least discuss blood glucose screening with a doctor if you have any of the common risk factors for diabetes, even if you don’t have any symptoms. As these risk factors include being over age 40, being overweight or obese, being physically inactive, having a family history of type 2 diabetes, having high blood pressure, having low HDL (good) or high LDL (bad) cholesterol levels, and being of African-American, Hispanic, Native American, Asian-American or Pacific Islander descent, “almost everyone” should be tested, Aloi said.
“I believe my job is to help people make correct choices, and to do that they need to have good information,” he said. “And part of that is screening for prediabetes and diabetes.”
Should testing reveal elevated blood glucose levels, the development of type 2 diabetes can in the majority of cases be prevented or delayed though lifestyle changes such as weight loss, healthier eating and increased physical activity. There are also anti-diabetes medications, such as metformin, which helps the body use insulin more efficiently.
“We can’t get rid of your genes or other things that may predispose someone to diabetes and we don’t have a cure, but we do know ways to control it,” Aloi said. “For most patients, especially if we’re catching prediabetes, the changes they need to make can be small but still effective.
“Losing 10 to 12 pounds and walking 20 minutes a day can be better than medicine. Sometimes restricting carbohydrates or adding more fiber to the diet helps a lot, and for younger patients simply eliminating sugary drinks might be enough.”
And while advanced type 2 diabetes can be also managed – or even put into remission – through treatment, the early identification of blood sugar problems is vital.
“You’re obviously better off preventing the complications from occurring than trying to treat them,” Aloi said. “I think it’s extremely important to identify the people who are at risk of diabetes and to tell them: This is the track you’re on. You should get out of the way of the train.”
Newswise —
E-cigarette use among teenagers is growing dramatically, and public health experts are concerned that these devices may be a gateway to smoking. Now, new research indicates that even if these young e-cigarette users do not become tobacco smokers, e-cigarettes may harm their health.In “Electronic-cigarette Use and Respiratory Symptoms in Adolescents,” published online ahead of print in the American Thoracic Society’s American Journal of Respiratory and Critical Care Medicine, lead author Rob McConnell, MD, professor of preventive medicine at the Keck School of Medicine at the University of Southern California, and colleagues report an association between e-cigarette use and persistent cough, bronchitis and congestion or phlegm in the Southern California Children’s Health Study. “E-cigarettes are known to deliver chemicals toxic to the lungs, including oxidant metals, glycerol vapor, diketone flavoring compounds and nicotine,” Dr. McConnell said. “However, there has been little study of the chronic health effects of e-cigarettes. The Children’s Health Study provided an opportunity to examine bronchitic symptoms common among smokers to see if the risk was also increased in users of e-cigarettes.” The researchers analyzed responses to a 2014 questionnaire completed by 2,086 study participants. Investigators categorized respondents as never e-cigarette users (76%), past users (more than 30 days earlier, 14.4%) and current users (at least once within the past 30 days, 9.6%). The study found that when compared to those who never tried e-cigarettes, the risk of the respiratory symptoms was
• approximately 85 percent higher among past users, and• double among current users
These associations remained statistically significant for past users after being adjusted for smoking and secondhand tobacco smoke exposure and sociodemographic factors. The researchers also looked at wheeze, a narrowing of the airways often caused by an asthma exacerbation, but did not find a significant association with e-cigarettes after adjusting for the same confounding factors.
“The Food and Drug Administration recently banned the sale of e-cigarettes to children under 18 years of age, and California just prohibited sale to young adults under 21,” Dr. McConnell said. “Our results suggest that these regulations and an environment that discourages the initiation of any tobacco product may reduce the burden of chronic respiratory symptoms in youth. However, because e-cigarettes are relatively new, additional study is needed to fully understand their long-term effects.”
Begun in 1992, the Southern California Children’s Health study has enrolled more than 11,000 children in one of the largest and most detailed studies of the long-term effects of air pollution on the respiratory health of children.
The National Institutes of Health and the Hastings Foundation funded this study.Contact for article: Rob McConnell, MD Via Zen Vuong, USC Media RelationsPhone: 213-300-1381Email: zvuong@usc.edu
Share via Twitter“Researchers find #e-cigarettes pose harm to teens beyond being gateway to smoking.”
Follow UsATS - @atscommunityAJRCCM - @ATSBlueEditor
About the American Journal of Respiratory and Critical Care Medicine (AJRCCM):The AJRCCM is a peer-reviewed journal published by the American Thoracic Society. The Journal takes pride in publishing the most innovative science and the highest quality reviews, practice guidelines and statements in pulmonary, critical care and sleep medicine. With an impact factor of 12.996, it is the highest ranked journal in pulmonology. Editor: Jadwiga Wedzicha, MD, professor of respiratory medicine at the National Heart and Lung Institute (Royal Brompton Campus), Imperial College London, UK.
About the American Thoracic Society:Founded in 1905, the American Thoracic Society is the world's leading medical association dedicated to advancing pulmonary, critical care and sleep medicine. The Society’s 15,000 members prevent and fight respiratory disease around the globe through research, education, patient care and advocacy. The ATS publishes three journals, the American Journal of Respiratory and Critical Care Medicine, the American Journal of Respiratory Cell and Molecular Biology and the Annals of the American Thoracic Society.The ATS will hold its 2017 International Conference, May 19-24, in Washington, DC, where world-renowned experts will share the latest scientific research and clinical advances in pulmonary, critical care and sleep medicine.
NEW STUDY FINDS CARDIOVASCULAR REHABILITATION HELPS REDUCE RISK OF DEATH IN DEPRESSED HEART PATIENTS
Newswise —
Depression has been known to be associated with poor cardiovascular outcomes, but if patients who are depressed attend cardiac rehabilitation after heart surgery, their risk of death is significantly reduced, according to a new study.
The study, conducted by researchers at Intermountain Medical Center Heart Institute in Salt Lake City, found that patients who were moderately to severely depressed had a higher risk of death after cardiovascular surgery than patients with mild to no depression. However, if those moderately to severely depressed patients attended rehabilitation after surgery, their risk of death was moderately reduced.
“We know the presence of moderate to severe depressive symptoms prior to cardiovascular surgery is a major risk factor for death, but our study shows that if those patients attend cardiac rehabilitation, their risk for death decreases significantly,” said the Intermountain Medical Center Heart Institute’s Viet Le, MPAS, PA, lead author of the study.
Results of the study will be presented at the 2016 American Heart Association’s Scientific Session in New Orleans on Sunday, November 13, at 5 pm, CST.
Le says several benefits of cardiac rehabilitation may play a role in reducing the risk for death in heart patients after cardiovascular surgery.
“We think cardiac rehab helps patients to manage their expectations as they return to work and life,” he said. “This comes from having a support group of fellow patients who may be further along in their rehab, as well as having exercise and activity protocols managed by experienced staff who can encourage consistent follow-up as well as ‘slow’ an overly enthusiastic patient. Getting patients out of their home after surgery, where they may overthink the effects of the disease, to a place where their job is to heal can enhance not only their physical recovery but their emotional health.”
The research indicates that patients who attend rehabilitation after surgery reduced their risk of death by nearly half, Le said, but further study is required to determine whether other factors contribute to this result, as well.
The Intermountain Medical Center Heart research team compiled information from 118 patients undergoing heart surgery who completed a nine-question patient health questionnaire (PHQ)-9 during an outpatient visit before their surgery.
Patients were categorized based on their results of their survey as having no to mild depressive symptoms or moderate to severe depressive symptoms. Following each patient’s completion of the last questionnaire, patients were followed post-surgery to determine the association of pre-surgery PHQ-9 depressive symptoms and death.
At the conclusion of the study, death occurred in 6.1 percent in patients with no to mild depressive symptoms and in about 25 percent of heart patients with moderate to severe depressive symptoms, showing that depressive symptoms were significantly associated with death.
Among patients with moderate to severe depression however, attending cardiac rehabilitation significantly decreased their risk of death by 74 percent (HR=0.26, p=0.02).
Other Intermountain Medical Center Heart Institute researchers involved in the study include: Tami L. Bair, Jose Benuzillo; Heidi T. May, PhD; Kirk U. Knowlton, MD; Donald L. Lappé, MD; and Joseph B. Muhlestein, MD.
Intermountain Medical Center is the flagship facility for the Intermountain Healthcare system, which is based in Salt Lake City.
###