News
Newswise —
About 20-25 percent of adults have the metabolic syndrome and have increased risk of developing both cardiovascular disease and type 2 diabetes. In this longitudinal study, investigators examined associations between childhood muscular fitness (strength, endurance, and power) and metabolic syndrome – the latter assessed once they reached adulthood. The results suggest that higher levels of childhood muscular fitness might protect against developing metabolic syndrome in adult years. Further, this relationship was found to be independent of the childhood cardiorespiratory fitness levels. For example, those with the highest muscular fitness at ages 9-15 years, had an 80 percent lower risk of developing metabolic syndrome in adulthood – in comparison to those who had low muscular fitness levels during childhood. Supporting the current World Health Organization physical activity guidelines, these results highlight the importance of both muscular strengthening activities and aerobic exercise. Overall, the study supports that a combination of increased muscular fitness, increased cardiorespiratory fitness and decreased adiposity in childhood may reduce future risk metabolic syndrome. Click here to access the abstract.
Newswise —
Hatha yoga is an increasingly popular form of physical activity and meditative practice in the U.S. It is important to understand the calorie cost and intensity of yoga in relation to the national physical activity guidelines, such as those recommended by the American College of Sports Medicine (ACSM) and the American Heart Association (AHA). These guidelines encourage 30 minutes of moderate-intensity physical activity on most days of the week. This study was a systematic review that evaluated published research investigations that have directly measured the calorie cost of yoga and calculated the metabolic intensity (METS) of individual yoga poses including a popular sequence called “sun salutations.” Based on ACSM/AHA classification, the intensity of holding most poses and of full yoga sessions ranged from light (less than 3 METS) to moderate-intensity (3-6 METS), with the majority classified as light-intensity. A few sequences/poses, including the sun salutations, met the criteria for moderate-intensity activity. The health benefits of yoga, however, should not be discounted. The regular practice of yoga may also increase strength, balance and flexibility, calm the mind and reduce stress. Click here to access the abstract.
Newswise — Washington, DC—
Exposure to bisphenol A (BPA) and other endocrine-disrupting chemicals (EDCs) may reduce levels of vitamin D in the bloodstream, according to a new study published in the Endocrine Society’s Journal of Clinical Endocrinology & Metabolism.
The study is the first to find an association between EDC exposure and vitamin D levels in a large group of U.S. adults.
EDCs are chemicals or mixtures of chemicals that can cause adverse health effects by interfering with hormones in the body. The Society’s Scientific Statement on EDCs examined more than 1,300 studies that found links between chemical exposure and health problems, including infertility, obesity, diabetes, neurological problems and hormone-related cancers.
“Nearly every person on the planet is exposed to BPA and another class of endocrine-disrupting chemicals called phthalates, so the possibility that these chemicals may even slightly reduce vitamin D levels has widespread implications for public health,” said the study’s first author, Lauren Johns, MPH, a PhD candidate at the University of Michigan School of Public Health in Ann Arbor, MI. “Vitamin D plays a broad role in maintaining bone and muscle health. In addition, low vitamin D levels have been implicated in outcomes of numerous conditions such as cardiovascular disease, diabetes and cancer.”
EDCs are found in everyday products and throughout the environment. There are more than 85,000 manufactured chemicals, of which thousands may be EDCs. BPA, a known EDC, is often found in plastics and other consumer products. Another group of chemicals linked to hormone disruption, phthalates, are found in personal care products such as cosmetics, children’s products, food packaging and medical tubing.The study examined data from 4,667 adults who participated in the National Health and Nutrition Examination Survey (NHANES) between 2005 and 2010. NHANES is a cross-sectional study designed to collect health and nutrition data from a sample of adults from across the United States. The participants provided blood samples so their vitamin D levels could be measured. To measure EDC exposure, the participants had their urine analyzed for substances left behind after the body metabolized phthalates and BPA.
The study found people who were exposed to larger amounts of phthalates were more likely to have low levels of vitamin D in the bloodstream than the participants who were exposed to smaller amounts of the EDCs. The link was strongest in women. There also was an association between exposure to higher levels of BPA and reduced vitamin D levels in women, although the relationship was not statistically significant in men.
“More research is needed into why an association exists, but it is possible that EDCs alter the active form of vitamin D in the body through some of the same mechanisms that they use to impact similar reproductive and thyroid hormones,” said Professor John D. Meeker, MS, ScD, senior author of the study. “Confirmatory studies are needed to show whether this association exists in other populations.”
The study, “Relationships between Phthalate and Bisphenol A Concentrations and Vitamin D Levels in U.S. Adults,” will be published online at http://press.endocrine.org/doi/10.1210/jc.2016-2134, ahead of print.
Kelly K. Ferguson of the University of Michigan School of Public Health and the National Institute of Environmental Health Sciences (NIEHS) in Research Triangle Park, NC, co-authored the study with Meeker and Johns.
The research was supported in part by the National Institutes of Health’s NIEHS, as well as its intramural research program.
For more information on endocrine-disrupting chemicals, visit the Endocrine Society’s centennial website.
# # #
Newswise — CHAPEL HILL –
An analysis of the quality of life of several thousand breast cancer survivors in North Carolina found differences in how black and white women functioned and felt physically and spiritually during treatment and two years after diagnosis.
The study, led by researchers from the University of North Carolina Lineberger Comprehensive Cancer Center, found white women reported higher physical and functional health-related quality of life scores compared with black women during active treatment. The gap in physical quality of life scores narrowed two years after diagnosis, however, and in both physical and functional measures after researchers adjusted the data to account for differences in education, insurance, and marital status. The findings suggest that improved socioeconomic conditions could enhance physical and functional quality of life for breast cancer survivors.
Yet, some differences remained. Chiefly, black women had higher spiritual quality of life scores five months and two years after diagnosis than white women, and after adjusting for socioeconomic factors.
“Black women generally had poorer physical and functional quality of life after the diagnosis of breast cancer, and socioeconomic and other factors explain some of these differences,” said study co-author Andrew Olshan, PhD, associate director of population sciences at UNC Lineberger and the Barbara Sorenson Hulka Distinguished Professor in Cancer Epidemiology at the UNC Gillings School of Global Public Health. “However, for some domains, black women report better quality of life.”
The study, published in the journal Breast Cancer Research and Treatment, drew upon surveys that assessed health-related quality of life issues for women aged 20 to 74 years who lived in North Carolina and had breast cancer. The analysis is part of the third phase of the Carolina Breast Cancer Study, a study first launched at UNC-Chapel Hill in 1993 as part of an effort to better understand why black women have been found to disproportionately die from breast cancer. Olshan is the co-principal investigator of the study.
Researchers used surveys to gauge the physical, functional, emotional and spiritual health-related quality of life of more than 2,100 women at five months after their breast cancer diagnosis, and at 25 months, when women have typically stopped active treatment and have entered the survivorship phase.For spiritual quality of life, researchers found that black women scored two points higher than white women at five months, when they were in the midst of active treatment, and two years after diagnosis. Specifically, black women scored an unadjusted average of 41.4 points on spiritual quality of life, while white women scored an average of 39.3 at five months. Two years after diagnosis, black women scored an unadjusted average of 40.5 on spiritual quality of life, while white women had an average score of 38.5. Even after adjusting for socioeconomic factors, black women continued to score higher than white women for spiritual quality of life two years after diagnosis, the study reports.
“Black women we surveyed had significantly better spiritual wellbeing than white women, and it was both statistically significant and clinically meaningful,” said the study's first author Laura Pinheiro, a doctoral candidate in the UNC Gillings School of Global Public Health.
White women’s average scores for physical and functional quality of life, which track women’s feelings of fatigue, nausea, pain, the woman’s ability to work, sleep, acceptance of her illness and ability to enjoy things in normal life, were two to 2.5 points higher than black women at five months. The unadjusted average score for white women’s physical health at five months was 20.9, compared to 18.4 for black women. For functional health, white women scored an average of 20.1 compared to 18.2 for black women.
At 25 months after diagnosis, the researchers found that white women still scored higher for physical, social, and functional health-related quality of life, but the gap between the unadjusted physical scores for white and black women narrowed compared to what they were at five months for physical health-related quality of life. Pinheiro said that the findings, in-line with previous studies, could suggest that the health care system may have had a positive impact on the black women’s overall physical health, helping to narrow those gaps.
“As these women are entering the health care system, perhaps some of their other health conditions are better managed,” Pinheiro said. “That is our speculation, and it will merit some additional investigation.”They also report that after adjusting for socioeconomic factors during survivorship, differences in physical health-related quality of life were diminished.
“Our research suggests that improved social and economic conditions could improve access to care, reduce co-morbid conditions, and other factors that are associated with both the prognosis of breast cancer, quality of life, and the disparities seen between various groups,” Olshan said.
The study demonstrates the importance of the Carolina Breast Cancer Study in understanding how breast cancer and its treatment impacts the lives of North Carolinians, said the study’s senior author Bryce Reeve, PhD, a UNC Lineberger member and professor in the UNC Gillings School of Global Public Health.“We hope to use these findings to find opportunities to improve the quality of life of women with breast cancer,” Reeve said.
In addition to Olshan, Pinheiro and Reeve, other authors included: Cleo A. Samuel, Katherine E. Reeder-Hayes, and Stephanie B. Wheeler.The study was supported by the University Cancer Research Fund of North Carolina, the National Cancer Institute Specialized Program of Research Excellence in Breast Cancer at UNC, the Susan G. Komen for the Cure Foundation, and the National Institutes of Health.
SEE ORIGINAL STUDY
Newswise —
Everyone knows that tobacco products are bad for your health, and even the new e-cigarettes may have harmful toxins. However, according to research at Texas A&M, it turns out the nicotine itself—when given independently from tobacco—could help protect the brain as it ages, and even ward off Parkinson’s or Alzheimer’s disease.
Ursula Winzer-Serhan, PhD, an associate professor at the Texas A&M College of Medicine, and her collaborators found that nicotine’s ability to be neuroprotective may be partly due to its well-known ability to suppress the appetite. Their research is published in the Open Access Journal of Toxicology.
Using animal models, Winzer-Serhan and her collaborators added nicotine to the animal’s drinking water. There were three different groups that received nicotine at three different concentrations (low, medium and high) corresponding to occasional, low and medium smokers, respectively, in addition to a control group that did not receive any nicotine.
The two groups that received nicotine at low and medium doses didn’t show any levels of the drug in their blood and they experienced no changes in food intake, body weight or number of receptors in the brain where nicotine acts. In contrast, the group getting the highest concentration of nicotine ate less, gained less weight and had more receptors, indicating that at higher doses, the drug gets into the brain where it can impact behavior. However, even at high doses, it didn’t seem to have worrying behavioral side effects like making the individuals more anxious, which the researchers were concerned could happen.
“Some people say that nicotine decreases anxiety, which is why people smoke, but others say it increases anxiety,” Winzer-Serhan said. “The last thing you would want in a drug that is given chronically would be a negative change in behavior. Luckily, we didn’t find any evidence of anxiety: Only two measures showed any effect even with high levels of nicotine, and if anything, nicotine made animal models less anxious.”
The next step is to test nicotine’s potential anti-aging effects using aged animal models. Although early results indicate that nicotine can keep older individuals from gaining weight like the control group does, Winzer-Serhan hasn’t yet determined whether this lower body mass index translates into less degeneration of the brain. It is also unclear if nicotine’s effects are related only to its ability to suppress appetite, or if there are more mechanisms at work.
Because there are still so many unknowns, Winzer-Serhan urges caution. “I want to make it very clear that we’re not encouraging people to smoke,” she said. “Even if these weren’t very preliminary results, smoking results in so many health problems that any possible benefit of the nicotine would be more than cancelled out. However, smoking is only one possible route of administration of the drug, and our work shows that we shouldn’t write-off nicotine completely.”
Still, Winzer-Serhan cautions people not to purchase nicotine-containing products just yet. “Although the results are intriguing, we would need large-scale clinical trials before suggesting anyone change their behavior,” she said. “At the end of the day, we haven’t proven that this addictive drug is safe—and it certainly isn’t during childhood or adolescence—or that the benefits outweigh the potential risks.”
Newswise —
A team of clinical scientists at the University of Bristol have found a new way to treat high blood pressure (hypertension). The research study, entitled “Unilateral carotid body resection in resistant hypertension: a safety and feasibility trial,” was led by Professor Julian Paton at the University of Bristol, and Dr Angus Nightingale (Cardiology Consultant) at the Bristol Heart Institute, Bristol, and was published recently in the Journal of American College of Cardiology: Basic to Translational Science.
The research indicates that the carotid bodies appear to be a cause of high blood pressure, and as such now offer a new target for treatment.
The clinical team have shown that removing one carotid body from some patients with high blood pressure caused an immediate and sustained fall in blood pressure.
Dr Nightingale said: “The falls in blood pressure we have seen are impressive – more than you would see with pharmacological medication – and demonstrate the exciting potential there now is for targeting the carotid body to treat hypertension.”
The carotid bodies “sniff” the levels of oxygen in blood, and when this falls they raise the alarm of a potential emergency by signaling to the brain to increase breathing and blood pressure. The effect is similar to having the thermostat in your home set too high all the time.
Professor Paton explained: “Treating the carotid body is a novel approach and a potential game changer as we believe we are reducing one of the main causes for hypertension in many patients. High blood pressure treatment typically tackles the symptoms targeting the end organs such as the heart, kidneys and blood vessels, and not the causes.”
“Most importantly, we have developed some unique tests to assess which patients have overactive carotid bodies. This now gives us a way to personalise treatment, which is essential as there are multiple reasons why high blood pressure develops” said Dr Nightingale.
The clinical trial demonstrated that the carotid bodies in patients who responded to resection had raised carotid body activity. These patients breathed more at rest and produced exaggerated breathing responses when the oxygen level in their blood was lowered.
High blood pressure is the world’s leading contributor to mortality. In the UK, its cost to the National Health Service is around £2 billion per year, and it remains poorly controlled, triggering heart and renal failure, and strokes. The World Health Organization has identified high blood pressure as the single most important risk factor for the global burden of disease and death.
“Although this surgical approach to controlling high blood pressure was successful, we don’t think this will be the solution in the long term. We now need to find a drug that dampens down an overactive carotid body and resets the blood pressure thermostat to a normal level,” Dr Nightingale said.
Professor Paton’s team may have found such an alternative. Recent animal studies published last week in Nature Medicine, discovered that the energy molecule adenosine tri-phosphate appears to be responsible.
“We are very excited by finding that we can turn down the alarm signals emanating from the carotid body in conditions of hypertension, yet it remains fully operational should an emergency situation occur. The new drug target we found within the carotid body is a receptor for the ATP molecule called the P2X3 receptor” explained Professor Paton.
Professor Paton said: “This approach may lead us to the first novel anti-hypertensive treatment strategy in more than 15 years. It has taken almost 10 years of research effort, working with colleagues from the University of Bristol, The University Hospitals Bristol NHS Foundation Trust, Medical University of Gdansk, Poland, the William Harvey Research Institute, London, Dartmouth Medical School, USA, the University of Sao Paulo, Brazil, the University of Auckland, New Zealand, Cibiem Inc., and Afferent Pharmaceuticals. Nor would it have been possible without funding from The British Heart Foundation.”
Paper
‘Purinergic receptors in the carotid body as a new drug target for controlling hypertension’ by Julian Paton et al in Journal of American College of Cardiology: Basic to Translational Science.
SEE ORIGINAL STUDY
Newswise —
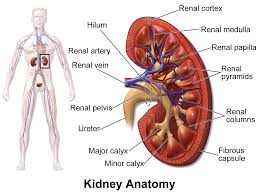
The increase in illnesses and deaths linked to medication-resistant bacteria has been well-documented by researchers and received extensive public attention in recent years. Now, UCLA-led research shows how these bacteria are making it more difficult to treat a common but severe kidney infection.
Pyelonephritis — infection of the kidney usually caused by E. coli bacteria and which can start as a urinary tract infection — causes fever, back pain and vomiting. About half of people infected require hospitalization. If not treated with effective antibiotics, it can cause sepsis and death.
In a UCLA-led study based on data from 10 large hospital emergency departments around the country, almost 12 percent of people diagnosed with pyelonephritis had infections resistant to the standard class of antibiotic used in treatment — fluoroquinolone. (Cipro and its generic version ciprofloxacin are commonly used medications in this class.) That’s up from 4 percent in a similar study conducted a decade ago. In some cities, and among some people with certain risk factors — such as international travel or recent hospitalization or treatment with an antibiotic — fluoroquinolone resistance rates exceeded 20 percent.
The new study — published in the September issue of Emerging Infectious Diseases — also documents the emergence of infections caused by a specific strain of E. coli that is resistant to additional types of antibiotics, severely limiting treatment options. That strain, dubbed ESBL for the antibiotic-destroying enzymes it produces (extended-spectrum beta-lactamases), was not detected in the previous study. The enzymes were first detected in 1979 and are most often found in developing nations.
Currently, there are only a few intravenous antibiotic options to treat ESBL-related infections, and no oral antibiotics that are consistently effective.
“This is a very real example of the threat posed by the emergence of new antibiotic-resistant strains of bacteria, which greatly complicates treatment of infection,” said Dr. David Talan, the study’s lead author and a professor in the department of emergency medicine at the David Geffen School of Medicine at UCLA. He is also a professor in the department of medicine, division of infectious diseases.
The study included 453 people diagnosed with kidney infection. The study participants were diagnosed between July 2013 and December 2014 in 10 emergency departments at large hospitals around the country, including Olive View–UCLA Medical Center in Sylmar, which is operated by Los Angeles County.
Researchers reported that:
- The rates of ESBL-related infections varied from 0 percent to more than 20 percent, depending on the location of the emergency room and patient risk factors.
- About one in three people infected with ESBL-producing E. coli had no traditional risk factors for antibiotic resistance, suggesting the bacterial strain is now endemic in the United States and healthy people are also at risk.
- About three of every four people infected with ESBL-producing E. coli were initially treated with antibiotics ineffective against that particular strain of bacteria, placing them at risk for poor outcomes.
Talan and his research colleagues recommended the development of new medications and new guidelines calling for treatment with different types and combinations of antibiotics. They also recommended physicians evaluating treatment options pay close attention to antibiotic resistance rates in their regions and quickly test bacteria samples to determine specific strains.
The research was supported by the U.S. Centers for Disease Control and Prevention and by Merck.
Newswise —
Cancer treatments that mobilize the body’s immune system to fight the disease have generated a lot of excitement in the past few years. One form of immunotherapy called checkpoint blockade is especially promising. But while checkpoint blockade has had some striking successes, the therapy has almost no effect on some of the most lethal kinds of tumors.
Now a group of scientists from the University of Chicago has developed an ingenious way to spur checkpoint blockade into more potent action. The therapy, reported in the Aug. 17 issue of Nature Communications, offers the hope of an effective treatment for intractable metastatic cancers including those of the colon and lung.
“Everybody out there working in the cancer space is trying to figure out ways to enhance checkpoint blockade immunotherapy,” said Wenbin Lin, James Franck Professor in Chemistry at UChicago and one of the scientists who conceived the new therapy. “In this work, we were able to achieve that.”
The method requires a complex interplay of immune-stimulating nanoparticles comprised of light-sensitive agents and standard chemotherapeutic drugs, both acting together to fortify the checkpoint blockade.
Bolstering immunity
Checkpoint blockade therapy works by interfering with cancer’s ability to turn off the body’s immune reaction. When cancer cells first develop, the body is able to recognize them as foreign, triggering T-cells to attack and eliminate them. But as malignant cells multiply and form tumors, they release biochemical signals that suppress the immune system and the T-cells no longer function properly.
Checkpoint blockade therapy obstructs those signals, makes T-cells see the cancer cells as invaders again, and allows the immune system to do its job. The problem, said Lin, is that if a tumor has been growing for years there are no longer any T-cells inside it to activate, so the therapy fails.
“So what we’re trying to do is to come up with ways to recruit T-cells to the tumor,” he said. “And if you have a way to make the T-cells recognize cancer cells, the T-cell will be able to go in there and kill the cancer cells.”
The treatment Lin and collaborators invented is a drug cocktail contained in a nanoparticle. The nanoparticles assemble themselves from zinc and a drug called oxaliplatin, which is widely used against advanced-stage metastatic colon cancer. A photosensitizing agent called pyrolipid forms the outer layer. When light is shined on the pyrolipid it generates molecules that can kill cancer. It also activates T-cells that can recognize cancer cells, so the nanoparticles pack a triple punch.
Used in concert, the nanoparticles and a checkpoint blockade agent were able to eliminate tumors in a mouse, even when the tumors were widely separated and one of them had received no treatment. The scientists injected a checkpoint blockade drug into the abdomen of a mouse that had two tumors growing at different places on its body, and then injected the nanoparticles into the mouse’s tail vein. They shined light onto one of the tumors to activate the pyrolipid. The other tumor was left untreated.
The irradiated tumor disappeared, as would be expected. But, remarkably, the distant, untreated tumor disappeared as well. No irradiation with light meant no T-cells were activated in the second tumor, “so we should not expect that tumor to disappear,” Lin said. “But we believe that this combination is able to activate the immune system to generate the T-cells that will recognize the cancer cells. Then they go around the body and kill the cancer cells in the distant site that has not been irradiated with the light.”
Traveling T-cells
This ability to activate T-cells in one place and have them travel to disease sites elsewhere in the body could be a powerful tool for treating cancer. Most people who die of cancer do not die from their primary tumor; they die from metastatic disease. When patients have surgery, surgeons don’t know if there are other, smaller lesions elsewhere in the body.
“You cannot treat them because you don’t know where to look for them,” Lin said. “If you activate immune cells, they can home in to cancer cells selectively. So you have a better chance of getting rid of these small metastatic tumors throughout the body.”
Lin and colleagues have started a company to develop the new therapy and have raised initial funding for clinical trials.
“These findings open up new opportunities for using nanoparticles as a platform for combination therapies,” said Yu-Ying He, an associate professor of medicine and dermatology at UChicago who is familiar with the work. “If the mouse models are indicative of human disease, the combination therapy can increase the proportion of patients who respond to therapy without additional adverse side effects and can improve the quality of life for cancer patients."—Carla Reiter
Citation: “Core-shell nanoscale coordination polymers combine chemotherapy and photodynamic therapy to potentiate checkpoint blockage cancer immunotherapy,” by Chunbai He, Xiaopin Duan, Nining Guo, Christina Chan, Christopher Poon, Ralph R. Weichselbaum, and Wenbin Lin, Nature Communications, published online Aug. 17, 2016, doi:10.1038/ncomms12499.
Funding: National Cancer Institute, University of Chicago Medicine Comprehensive Cancer Center, Cancer Research Foundation, and Ludwig institute for Metastasis Research.
Newswise —
A UC Santa Barbara researcher studying how the brain uses perception of the environment to guide action has a new understanding of the neural circuits responsible for transforming sensation into movement.
“Mapping perception to a future action seems simple,” UCSB neuroscientist Michael Goard. “We do it all the time when we see a traffic light and use that information to guide our later motor action. However, how these associations are mapped across time in the brain is not well understood.”
In a new paper, published in the journal eLife, Goard and colleagues at the Massachusetts Institute of Technology make progress in mapping brain activity in mice during simple but fundamental cognitive tasks. Although a mouse’s brain is much smaller than a human’s, remarkable structural similarities exist. The mouse brain is composed of about 75 million nerve cells or neurons, which are wired together in complex networks that unerlie sophisticated behaviors.
The researchers used large-scale calcium imaging to measure the responses of individual neurons in multiple areas of the brain while mice performed a delayed response task. First, they trained mice to respond to visual stimuli — drifting bars — by either licking or withholding licking, depending on whether the bars moved vertically or horizontally. While the mice performed the task, the investigators recorded neural activity from multiple brain regions thought to be involved — including visual, parietal and frontal motor cortices.
Using a powerful laser-scanning microscope, the team was able to detect the signals from calcium indicators expressed in the neurons well below the brain’s surface. Neurons normally have very low concentrations of intracellular calcium, but when they become active, calcium levels rise, increasing the fluorescence of the indicator and enabling measurement of neuron activity. In this way, the scientists were able to see which neurons were active while the mice performed the delayed response task.
“As expected, we found many neurons that responded only during the visual stimulus or the licking action, but we also found a lot of neurons that responded during other parts of the task,” said Goard, an assistant professor in UCSB’s Department of Psychological & Brain Sciences and Department of Molecular, Cellular and Developmental Biology. “In the frontal motor cortex, we found quite a few neurons that were active during the delay period between the visual stimulus and motor response. This led us to several new interpretations of the role that different brain regions were playing during performance of the task.”
Based on the neural activity in the different brain areas, Goard and his team then used optogenetics — a method of manipulating the nerve cells with light — to inactivate neurons in a temporally precise manner to identify those that function during different parts of the task. This allowed them to figure out which areas were necessary for performing the task. For example, the team determined that the visual and parietal areas are involved in perceiving the stimulus and transforming that into a motor plan, but only the frontal motor cortex is necessary for maintaining the motor plan over the delay period.
“Using this general approach, we hope to map the essential regions for different types of cognitive tasks,” Goard explained. “We are particularly interested in how mice maintain specific types of memories across distributed brain regions.”
SEE ORIGINAL STUDY
Newswise — PHILADELPHIA—
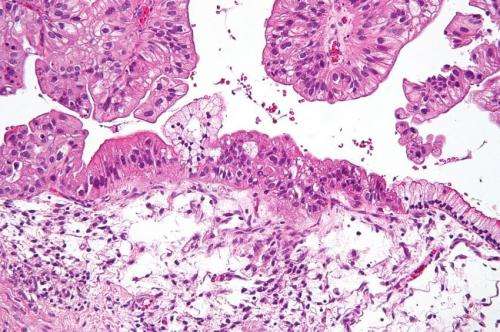
Few effective treatments have been approved to treat ovarian cancer, the deadliest of all cancers affecting the female reproductive system. Now, new research from The Wistar Institute demonstrates how a drug already in clinical trials could be used to boost anti-tumor immunity and cause T-cells to target the cancer directly while minimizing side effects. The results were published in the journal Cell Reports.
There has been considerable interest in the programmed cell death-1 (PD-1) protein and its ligand (PD-L1) because the interaction between the two inhibits important T-cell activity aimed at stopping tumor growth. PD-L1 is expressed on the surface of both cancer cells and immune cells across many different cancer types. Antibody-based drugs that specifically halt this interaction have shown promising results, though patients have experienced immune-related side effects as a result.
“We wanted to explore anti-PD-L1 therapies specifically for ovarian cancer, but we also wanted to determine if other drugs that did not cause these negative anti-PD-L1 antibody-related side effects could be used to target this cancer-promoting pathway,” said Rugang Zhang, Ph.D., professor and co-program leader in the Gene Expression and Regulation program at The Wistar Institute and lead author of the study.
Zhang and his team decided to screen for small molecule inhibitors that could be used as a treatment option. Small molecule inhibitors are a preferable form of cancer treatment because they block cancer progression by targeting cells that have proteins or mutations associated with cancer while sparing normal, healthy cells.
The researchers found that a class of drugs known as bromodomain and extraterminal domain (BET) inhibitors were particularly effective at suppressing PD-L1 activity when they studied the drug in epithelial ovarian cancer cell lines. Multiple BET inhibitors are in various stages of clinical trials for different types of cancer. They are able to suppress inflammatory responses, and they may be able to do so without affecting the anti-tumor immune response. In this study, they used an experimental BET inhibitor called JQ1.
Even though BET inhibitors do not specifically target PD-L1, the researchers were able to determine why this class of drugs is so effective. They showed that bromodomain-containing protein 4 (BRD4), one of the members of the BET family that is inhibited by these drugs, is a critical regulator of PD-L1 expression. The BRD4 gene is often amplified in ovarian cancer and may serve as a valuable biomarker to determine which ovarian cancer patients could benefit the most from receiving treatment with BET inhibitors.
“Targeting PD-L1 appears to be an effective strategy for combating a variety of human cancers,” said Hengrui Zhu, Ph.D., a postdoctoral fellow in the Zhang lab and first author of the study. “With BET inhibitors, we believe we have found a powerful new addition to available therapeutic strategies for ovarian cancer.”
This work was supported by the National Institutes of Health/National Cancer Institute R01 grants CA160331, CA163377, CA202919 and K99CA194318, U.S. Department of Defense grants OC140632P1 and OC150446, an Ovarian Cancer Research Fund (OCRF) program project and The Jayne Koskinas & Ted Giovanis Breast Cancer Research Consortium at Wistar. Zhu is an OCRF Ann Schreiber Mentored Investigator. Support for shared resources used in this study was provided by Cancer Center Support Grant (CCSG) CA010815 to The Wistar Institute. The Structure Genomics Consortium provided the panel of small molecule inhibitors that target epigenetic regulators used in this study.
Co-authors of this study from The Wistar Institute include Fee Bengsch, Nikolaos Svoronos, Melanie Rutkowski, Benjamin Bitler, Michael Allegrezza, Yuhki Yokoyama, Andrew Kossenkov, and José Conejo-Garcia. James Bradner from Dana-Faber Cancer Institute was also a co-author of this study.
###